90% Acute Lymphoblastic Leukemia Patients See Remission After Receiving Personalized Cellular Therapy
It sounds like something out of a sci-fi movie. You develop soldiers with genetic superpowers and then unleash them on the enemy to track and destroy them. Only it's not a movie but a life-saving new investigational personalized cellular therapy, called CTL019, that has brought hope to terminally ill adults and children by sending their acute lymphoblastic leukemia (ALL) into remission.
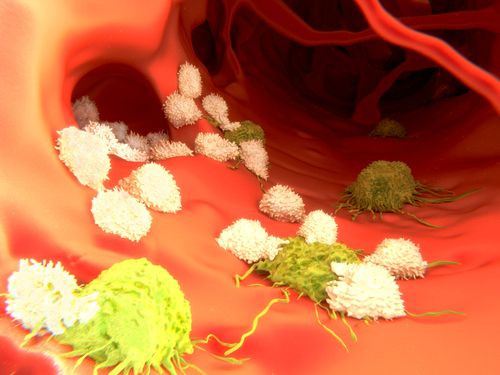
The therapy, developed by the Perelman School of Medicine at the University of Pennsylvania, involved infusing patients with genetically engineered "hunter" cells that tracked and systematically destroyed tumor cells.
"The patients who participated in these trials had relapsed as many as four times, including 60 percent whose cancers came back even after stem cell transplants. Their cancers were so aggressive they had no treatment options left," said lead author Stephan Grupp in a press release.
The responses achieved by the therapy have been unprecedented, he says, stating that after the therapy, 27 of the 30 patients in the studies achieved a complete remission and 78 percent of the patients were alive six months after treatment. The results of the therapy are published the The New England Journal of Medicine.
The soldiers — that is, the patient’s own T cells — were collected from their blood and then reprogrammed in Penn's Clinical Cell and Vaccine Production Facility. This reprogramming involved a gene transfer that helps T cells identify and kill tumor cells. The modified T cells contain an antibody-like protein known as a chimeric antigen receptor (CAR), which is designed to bind to a protein called CD19 found on the surface of normal and cancerous B cells, responsible for several types of leukemia.
The modified T cells, called "hunter" cells by the team, are then infused back into the patient’s blood stream where they multiply and attack the tumor cells. A specialized signal built into the CAR encourages rapid growth to build a lean, mean fighting machine against the cancer. Tests have shown that each single engineered cell can generate more than 10,000 new cells.
The patients were in the age group of 5 to 60. Nineteen of the 30 continue to remain in remission, of which 15 have received only this therapy. This includes a 9-year-old who received the therapy more than two years back. Seven patients relapsed, between six weeks and 8.5 months after their infusions, including three whose cancers returned as CD19-negative leukemia.
All patients who had been infused with the "hunter" cells experienced a cytokine release syndrome (CRS) within a few days following the therapy, an indication that the cells had begun multiplying and killing tumor cells in the body.
Twenty-two of the 30 patients showed moderate effects of the CRS that included high fevers, nausea, and muscle pain — basically flu-like symptoms. Eight patients developed severe CRS and needed treatment for low blood pressure and breathing problems. Some other side effects were also observed that needed administration of immunosuppressant drugs or short courses of steroids, but eventually all patients recovered from CRS.
Blood tests of patients in complete remission revealed that the "hunter" cells were also destroying normal B cells that expressed CD19 protein. In other words, the modified T cells were working like vaccines, providing long-term protection against tumor recurrence.
"Our results support that CTL019 can produce long-lasting remissions for certain heavily pretreated ALL patients without further therapy," said coauthor Noelle Frey. "For our patients who have already relapsed after stem cell transplants, or don't have any options for donors, this option has provided new hope."
The therapy got much deserved recognition when in July this year the FDA granted the CTL019 its Breakthrough Therapy designation for the treatment of relapsed and refractory adult and pediatric ALL.
This recognition will aid in developing new medicines to treat life-threatening cancers, say the authors.
Source: Frey N, Grupp S, June C. New England Journal of Medicine. 2014.



























