Antibiotic Resistance Breakthrough: New Treatment Prevents Bacterial Skin Infections
English scientists may have hit upon a novel way of fighting off antibiotic-resistant superbugs: Turning our skin into the equivalent of a Slip 'N Slide.
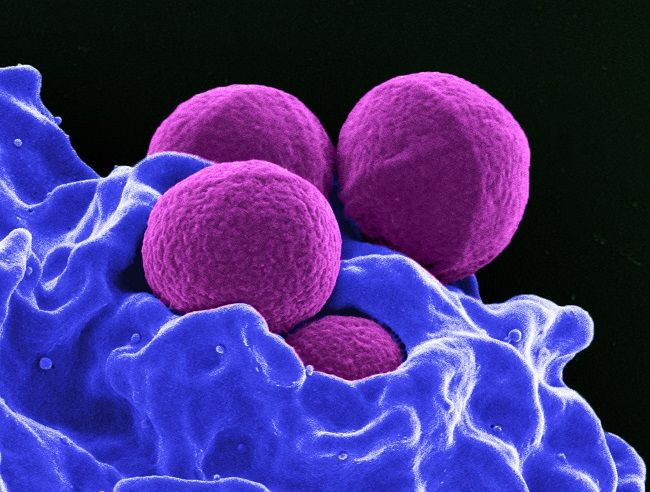
Researchers at the University of Sheffield have developed an experimental treatment designed to protect skin wounds from being infected by various multidrug-resistant strains of Staphylococcus aureus. Rather than attacking the germs, however, the treatment instead makes it harder for them to attach to our skin cells in the first place. In experiments with cultured skin cells and a 3D tissue-engineered model of injured skin, the treatment reduced the bacteria’s stickiness to cells by 50 to 60 percent when compared to a control. Importantly, the treatment didn’t appear to interfere with the skin cells’ natural healing process, meaning it may be perfectly harmless to real people. The results of their trial were published recently in PLOS-One.
"This development is a huge breakthrough in the fight against antibiotic-resistance,” said senior author Dr. Pete Monk of the University’s Department of Infection, Immunity and Cardiovascular Science in a statement.
The treatment is derived from a class of proteins that already play a vital role within our human bodies called tetraspanins. Tetraspanins are located in the cell membrane and, among many other responsibilities, help cells stick to surfaces or other cells. They do so by joining together with other parts of the cell, including other tetraspanins, and forming structures called tetraspanin-enriched microdomains. Unfortunately, certain bacteria, viruses, and protozoans can also manipulate these structures to stick themselves to cells and gain entry within, including HIV.
To come up with their treatment, the researchers tested out specific compounds, or peptides, from one of these structures previously shown in the lab to short-circuit the stickiness of many bacterial species. One peptide in particular, Peptide 800, proved especially effective in making skin cells non-sticky. And because these peptides don’t harm or kill bacteria, it’s less likely that they will encourage further drug resistance.
Skin infections are already a big worry within hospitals, a premier hotspot of superbugs, and the researchers are hopeful their treatment can be an especially important tool in preventing open wounds caused by surgery and bed sores from becoming infected.
"We hope that this new therapy can be used to help relieve the burden of skin infections on both patients and health services while also providing a new insight into how we might defeat the threat of antimicrobial drug resistance,” said Monk. “The therapy could be administered to patients using a gel or cream and could work well as a dressing. We're hoping it can reach clinical trials stage in the next three to five years."
Though the potential of tetraspanin-related therapies is obviously exciting, it’s still in the very early stages. Among one of the stumbling blocks, as mentioned earlier, is that the therapy only partially reduced bacteria’s sticking power. That suggests there might be other ways these bacteria manage to stick to us, and it’s likely the treatment may not work as effectively when applied to different types of cells (keratinocytes, which the peptides were most effective on, make up our outer skin). Given their ability to work against different species of bacteria and their low toxicity, though, the authors believe the sky’s the limit for these nifty little peptides.
Source: Ventress J, Partridge L, Read R, et al. Peptides from Tetraspanin CD9 Are Potent Inhibitors of Staphylococcus Aureus Adherence to Keratinocytes. PLOS One. 2016.



























