Blood-Brain Barrier Opened For The First Time In Human Patients In Cancer Breakthrough
Two of the most aggressive forms of neurological illness, Alzheimer’s disease and brain cancer, may see tougher fights now that scientists have opened up the blood-brain barrier in humans for the first time.
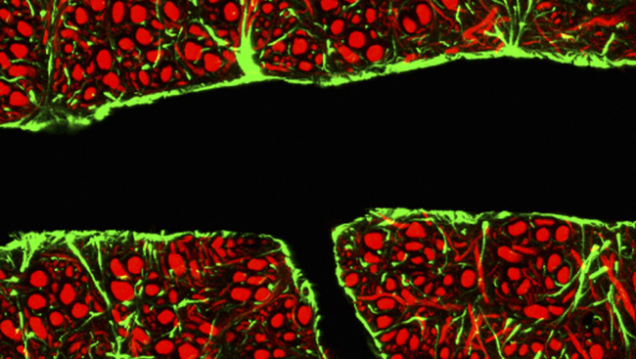
The surgery is already being hailed as a breakthrough. Considered the “front frontier” in neuroscience, the blood-brain barrier is the sheath of cells that separates the organ from the rest of the body. While it stops harmful toxins in the blood from hijacking vital tissues, it also prevents helpful drugs from rooting out tumors and disease. But now scientists say all that could change.
Four patients made up the focus of the study, carried out by neuroscientist Michael Canney and his colleagues at the Paris-based medical start-up CarThera. Each patient was getting treated for glioblastoma, the most aggressive type of brain tumor. Normally, patients with this type of cancer undergo surgery to have the tumor removed, then chemotherapy to remove any remaining cancer cell traces. But this method is imperfect, since it relies on a closed barrier.
Under normal circumstances, the blood-brain barrier lets through virtually no drugs into the brain — the ideal target, because that’s where the cancer lives. If more of the chemotherapy drugs could get through, they’d do a better job of killing cancer, Canney says. So he and his team set to exploring that possibility.
Using a hole in the patients’ skulls, which measured no more than 10 millimeters by four millimeters and had already been used for eliminating brain tumors, doctors inserted a tiny ultrasound brain implant. They also injected a supply of microbubbles. When the pulses emitted by the ultrasound hits the bubbles, it causes them to vibrate. This in turn pries open the cells of the blood-brain barrier.
Canney estimates the tandem approach helps keep the barrier open for up to six hours, during which time they can supply the patient’s brain with far greater drug dosages than when it was closed. A follow-up MRI scan showed a marker chemical that was injected along with the bubbles (as a way to track permeability), was smoothly crossing the blood-brain barrier.
"We hope this means the chemotherapy drug is doing the same thing," said Canney, who presented the team’s observations recently at the Focused Ultrasound symposium in Bethesda, Md. It will still be several months before the researchers can test the method on tumors, Canney concedes.
In the meantime, they’ll continue looking at the interaction between Alzheimer’s disease and amyloid protein plaques. The leading theory in Alzheimer’s research suggests that an overabundance of misfolded proteins disrupts neural connections. When these neurons can’t talk to one another, normal processes like memory lose their function. Canney suspects that merely opening up the barrier, even without introducing drugs, liberates the immune system to fight back.
“We think we will have a significant effect on these tumors,” Canney said.



























