Breakthrough In Fibromyalgia Research: Pain Is In Your Skin, Not In Your Head
Fibromyalgia has been a mysterious disease, causing pain throughout the body and deep in tissues with no apparent cause. A large proportion of the medical community has believed that the disease was psychosomatic, and people essentially think that they are in pain. But a small biopharmaceutical company, Intidyn, or Integrated Tissue Dynamics, has found what they believe to be the root cause of the disease.
Reseachers from the company and from Albany Medical College have found that there is a unique neurovascular structure, or blood flow to the nerves, in the skin of female patients who report pain from fibromyalgia. This, the scientists believe, may be the ultimate cause of the pain experienced in the condition.
"Instead of being in the brain, the pathology consists of excessive sensory nerve fibers around specialized blood vessel structures located in the palms of the hands," said Dr. Frank L. Rice, president of Intidyn and the senior researcher on the study, in a press statement
"This discovery provides concrete evidence of a fibromyalgia-specific pathology which can now be used for diagnosing the disease, and as a novel starting point for developing more effective therapeutics."
A few years ago, the company published a report in the journal Pain about a case involving a woman who was born without special nerve endings that were at the time believed to be important for touch. But the woman was fine and able to carry on with her life. She did have nerve endings near the fine capillary blood vessels in her skin, which had previously only been believed to control blood flow in blood vessels. "We previously thought that these nerve endings were only involved in regulating blood flow at a subconscious level, yet here we had evidence that the blood vessel endings could also contribute to our conscious sense of touch... and also pain," Rice said.
Current targeted drugs, made by Eli Lilly and Forest Labs, are serotonin/norepinephrine reuptake inhibitors (SNRI) that work on the brain. But, they can also act on the nerve endings near blood vessels in the skin. "Knowing how these drugs were supposed to work on molecules in the brain," Dr. Philip J. Albrecht, Ph.D., added, "we had evidence that similar molecules were involved in the function of nerve endings on the blood vessels. Therefore, we hypothesized that fibromyalgia might involve a pathology in that location." As the results demonstrate, they were correct.
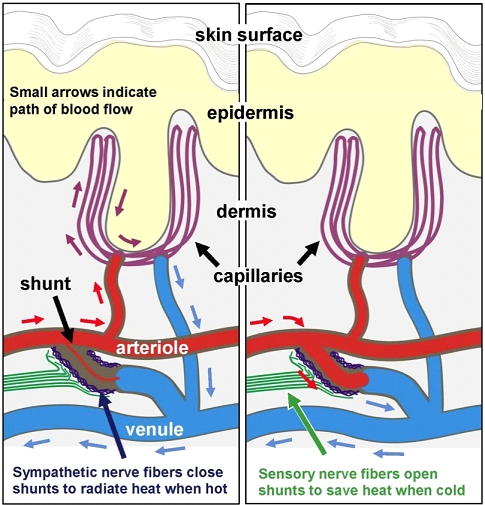
The research team at the company looked at skin samples from women with fibromyalgia collected by the Albany Medical College and examined by a special microscope technology. What they saw was a staggering increase in nerve endings at the site of blood vessels within skin. These sites control the flow of oxygenated blood between small blood vessels within the skin. They can cause the blockage of this bridge area to allow the skin to radiate heat or open it up to keep heat in when cold.
"The excess sensory innervation may itself explain why fibromyalgia patients typically have especially tender and painful hands. But, in addition, since the sensory fibers are responsible for opening the shunts, they would become particularly active under cold conditions, which are generally very bothersome to fibromyalgia patients," said Albrecht.
But these special shunts or bridges do much more than regulate heat in the body; they could be blocking blood flow to the muscles deep within the tissue.
"In addition to involvement in temperature regulation, an enormous proportion of our blood flow normally goes to our hands and feet. Far more than is needed for their metabolism," noted Dr. Rice. "As such, the hands and the feet act as a reservoir from which blood flow can be diverted to other tissues of the body, such as muscles when we begin to exercise. Therefore, the pathology discovered among these shunts in the hands could be interfering with blood flow to the muscles throughout the body. This mismanaged blood flow could be the source of muscular pain and achiness, and the sense of fatigue which are thought to be due to a build-up of lactic acid and low levels of inflammation fibromyalgia patients. This, in turn, could contribute to the hyperactvity in the brain." The hyperactivity in the brain may account for the insomnia many patients with the condition experience.
Finding an actual physiological basis for fibromyalgia will be a positive revelation for many who have been told that their pain is only in their head. With time, researchers will be able to further dissect the causes for the pain in the disease and may develop pharmaceuticals to deal with the actual cause of the pain.
A patient-friendly press release can be found here.
Source: Albrecht P, Hou Q, Argoff C, Storey J, Wymer J, Rice F. Excessive Peptidergic Sensory Innervation of Cutaneous Arteriole-Venule Shunts (AVS) in the Palmar Glabrous Skin of Fibromyalgia Patients: Implications for Widespread Deep Tissue Pain and Fatigue. Pain Medicine. 2013.



























