Common Surgeries, Including Hernia Repair, Are Safer And Less Expensive In Rural Hospitals

“Practice makes perfect.” Most of us understand this saying to be true in our own lives, so we tend to apply this reasoning to other, more complex situations that we may not understand so well. For instance, many people believe a higher-traffic hospital is more likely to be a well-oiled, functioning machine that can provide us with the safest overall care when it comes to surgery. A new study, however, suggests this perception is not entirely accurate.
When it comes to common operations, say University of Michigan researchers, so-called “critical access” hospitals in rural locations provide a safer and less expensive experience than suburban or city hospitals. The designation has been given to certain remote hospitals by the Centers for Medicare and Medicaid Services to improve access to health care and keep essential services within out of the way communities. These hospitals are the closest option for tens of millions of Americans.
For the study, the research team analyzed data from 1.6 million hospital visits, comparing what happened to patients at 828 critical access hospitals with data from patients at more than 3,600 larger hospitals. Specifically, the scientists focused on Medicare patients undergoing four common operations: gallbladder removal, colon surgery, hernia repair, and appendectomy.
While the risk of dying within 30 days of the operation was the same across all hospitals, they discovered the risk of suffering a major complication after surgery was lower at critical access hospitals compared to larger facilities. Complications included heart attacks, pneumonia, and kidney damage. Importantly, the researchers discovered patients who had these operations at critical access hospitals checked in healthier to begin with, suggesting that surgeons in these remote hospitals are appropriately selecting patients who will do well in a small rural setting while triaging more complex patients to larger centers.
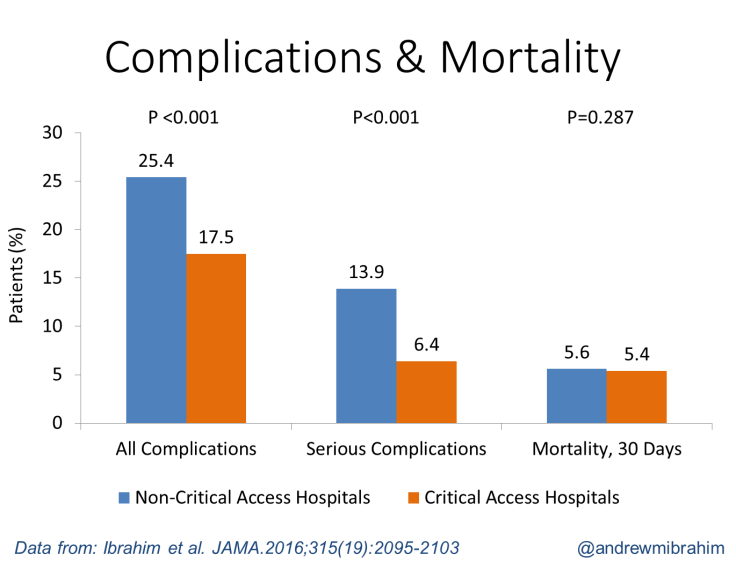
However, even after correcting for differences in pre-operation health, lead author Dr. Andrew Ibrahim and his co-researchers discovered the critical access hospitals still had equal or better outcomes. Similarly, after factoring in risk and payment differences, patients undergoing an operation at a critical access hospital cost the Medicare system nearly $1,400 less than patients who had the exact same surgery at a larger hospital.
The Underdogs
Critical access hospitals, which are located more than 35 miles from another hospital, provide 24/7 emergency care services. They have 25 or fewer acute care inpatient beds and maintain an annual average length of stay of 96 hours or less for acute care patients. Congress created the critical access hospital designation following a string of hospital closures in the 1980s and early 1990s to reduce continued shut-downs. Essentially, instead of standard reimbursement rates, Medicare pays slightly more than the total cost of care for procedures performed in these hospitals. Despite this boost, hundreds of these hospitals are in danger of closing, and this has spurred a national debate that’s currently underway.
Though they may be necessary to people living in rural locations, two recent critical investigations suggested these hospitals may not be serving patients well. One 2011 investigation found critical access hospitals had fewer capabilities and higher mortality rates for patients suffering a heart attack, congestive heart failure (a chronic condition where the heart doesn’t pump blood as it should), or pneumonia compared to larger hospitals. Another 2013 study indicated conditions at these smaller hospitals may have worsened over time; an examination of 30-day mortality rates at critical access hospitals showed an increase relative to larger hospitals between the years 2002 and 2010.
The current report, then, exclusively examined surgical care at these rural hospitals and gave them high marks. Among the positive surgical findings, the researchers discovered critical access hospital patients were less likely to require nursing facilities after their operations. And, less than 5 percent of surgery patients got transferred to larger hospitals, compared with more than a quarter of patients treated for non-surgical issues.
The study’s limitations include the possibility that the research team may have overestimated complication rates at larger hospitals due to how administrative reports code data. Still, the results indicate these hospitals perform well and safely at least from a surgical standpoint. Ibrahim and his co-researchers believe the implications of their work are significant to Medicare policies.
Source: Ibrahim AM, Hughes TG, Thumma JR, Dimick JB. Association of Hospital Critical Access Status with Surgical Outcomes and Expenditures among Medicare Beneficiaries. JAMA. 2016.
Published by Medicaldaily.com



























