Crohn’s Disease Severity Depends On Type Of Immune Cells Behind Patient’s Inflammation
New hope for drug development in the fight against Crohn’s disease, one of two burdening inflammatory bowel diseases, has emerged from a recent study that found which immune cells determine the severity of a patient’s disease.
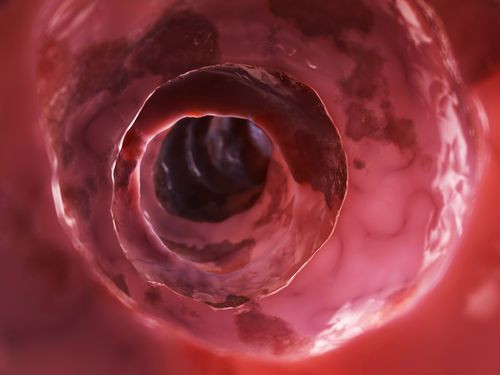
Though it’s often mistaken for an auto-immune disease, Crohn’s does affect people’s immune systems — attacking otherwise healthy tissue thinking it needs protection. The result is an inflamed portion, of undetermined length, in a person’s gastrointestinal tract. There is no cure for the disease, and little can be done to effectively screen for it. Some 1.4 million people in the U.S. suffer from inflammatory bowel diseases, according to the CDC, and many experts expect the numbers to rise as the country stays hell-bent on sterility and sanitization.
The present study focused on immune cells known as microphages, whose primary role is to engulf and digest harmful pathogens in the blood. Researchers used both blood macrophages and intestinal macrophages, dividing both into three subsets. When they tested each one on both healthy subjects and those diagnosed with Crohn’s, they found one in particular, known as (ahem) CD14hiHLA-DRdim macrophages, resulted in the greatest inflammation.
"By increasing the knowledge on the different macrophage subsets in the intestine and their blood counterparts, we hope to contribute to the discovery of more specific targets in Crohn's disease, increasing the efficiency of new treatments,” Dr. Olof Grip, a researcher from the Department of Clinical Sciences Malmö at Lund University, said in a statement.
Now that the team has the specific cells pinned down, they hope they can use the information to develop targeted drugs that rely on alternative pathways for treatment. As it stands now, Crohn’s patients typically receive either immunosuppressant drugs, which stop the body from making destructive mistakes against itself; take anti-inflammatory steroids; or, in the most extreme cases, undergo surgery to remove the destroyed tissue.
"This work provides new leads for drugs and therapeutic targets for Crohn's disease and possibly other conditions that involve runaway inflammation," said Dr. John Wherry, deputy editor of the Journal of Leukocyte Biology, where the study was published. "Most of our therapies for intestine inflammatory diseases like Crohn's involve non-specific immunosuppression that have variable efficacy and many side effects.”
Patients who require heavy doses of this medicine put themselves at risk for other illnesses, as their body's defenses are weakened from treatment. It’s critical, then, to develop a way of controlling inflammation without cutting the immune system’s legs out from under it completely. Wherry, for one, expresses hope. “These new studies suggest that targeting specific cell types could increase the ability to specifically treat disease, reduce unwanted side effects, and hopefully,” he said, “help people lead healthier lives."
Source: Thiesen S, Janciauskiene S, Uronen-Hansson H, et al. CD14hiHLA-DRdim macrophages, with a resemblance to classical blood monocytes, dominate inflamed mucosa in Crohn's disease. Journal of Leukocyte Biology. 2014.
Published by Medicaldaily.com



























