Effects Of Poverty Impact Gene Expression In The Brain, Leading To Depression: Study
Various studies link poverty and depression. At the same time, a growing body of scientific research shows how biological factors also lead to symptoms of depression. Duke University researchers combined behavioral data with genetics and brain imaging to show how poverty can lead to biological changes — in this case, gene expression — in the brains of teenagers. The altered genetic expression influenced the teens’ cognitive development, which in turn led to depressive symptoms as they grew older.
The researchers examined how chemical tags that influence expression of a gene, known as SLC6A4, changed over time. Essentially, every gene contains a set of instructions to code for specific proteins (or other cell products), yet the amount of protein a gene is able to make can be modified by other genes and other processes. Since proteins are the workhorses of a cell, the number and type of proteins made will impact cellular function and ultimately shape the organism itself.
“We focused on SLC6A4, which encodes the serotonin transporter, because we already know a good deal about the importance of this gene and this molecule on stress-related amygdala function and behavior,” Dr. Ahmad Hariri, a professor of psychology and neuroscience at Duke, told Medical Daily in an email.
From Gene Expression to Depression
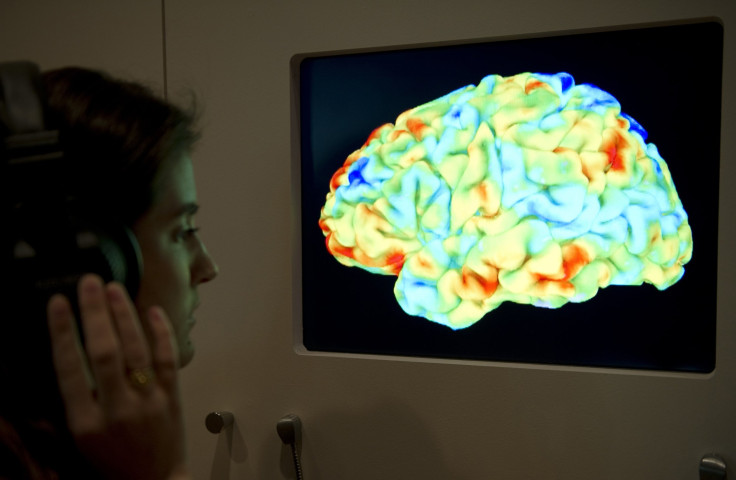
Serotonin is a chemical that transmits signals in the brain; this neurotransmitter has been linked to mood disorders, including depression. The gene SLC6A4 helps control levels of serotonin throughout the brain, including within the amygdala, an almond-sized region commonly believed to be the source of primal emotions. In a previous study, Hariri and his colleagues demonstrated the amygdala becoming more active in the presence of threats; for instance, when study participants viewed aggressive-looking faces, their brain scans showed the amygdala “lighting up” in response.
Building on this for the current study, Hamiri and his team focused on the process known as “methylation,” where chemical tags are attached to a stretch of DNA near the SLC6A4 gene. The more tags present, the less likely this gene will be active and the less control it will have over the flow of serotonin, a mood regulator, in the brain.
For the study, then, Hariri and his colleagues looked at possible changes in these chemical tags in the brains of teens over time to understand how this might influence depression. A total of 132 non-Hispanic white teens participated in the study. They came from households ranging from low to high socioeconomic status, and about half had a family history of depression. At the start of the study, the teens were between 11 and 15 years old. In successive waves over the course of three years, the researchers collected information on the teens. Not only did the teens undergo brain scans but they also completed psychological assessments.
What did Hariri and his team discover when they analyzed their results? Teens growing up in impoverished households accumulated, over the course of three years, greater quantities of the chemical tag on SLC6A4, the depression-linked gene. The tags altered genetic expression in such away that the more tags, the more each teen’s amygdala responded to aggressive faces (as seen during a brain scan). Importantly, teens with the most active amygdalas were more likely to report symptoms of depression as they grew older.
Though this research is preliminary, the results demand further testing. According to lead author Johnna Swartz, the team is now searching for new markers of genetic changes, since an entire panel of markers would naturally lead to more accurate predictions of depression.
“This is some of the first research demonstrating that low socioeconomic status can lead to changes in the way genes are expressed,” said Swartz. “And it maps this out through brain development to the future experience of depression symptoms.”
Source: Swartz JR, Hariri AR, Williamson DE. An Epigenetic Mechanism Links Socioeconomic Status to Changes in Depression-Related Brain Function in High-Risk Adolescents. Molecular Psychiatry. 2016.
Published by Medicaldaily.com