Human Gene, MX2, Could Prevent HIV From Spreading Once It Enters The Body
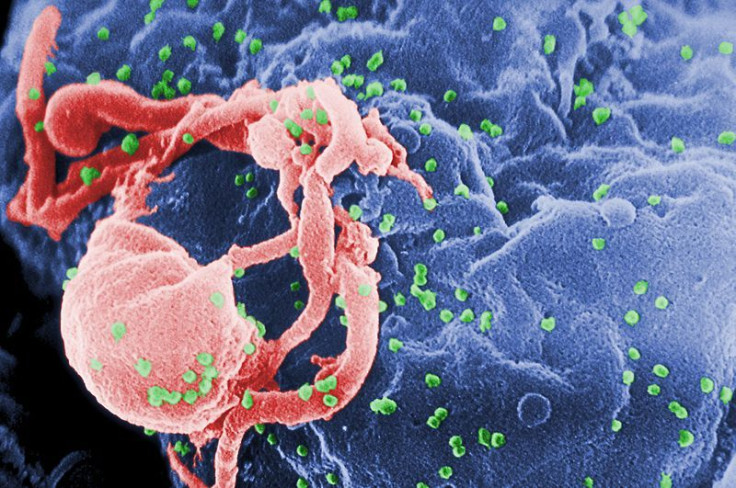
A study published this week in Nature has identified a gene which may have the ability to prevent human immunodeficiency virus (HIV) from spreading once it has entered the body. Researchers from King’s College London say the human MX2 gene, which possibly inhibits HIV, the virus that causes acquired immune deficiency syndrome (AIDS), could be a new target for effective, less toxic treatments for patients.
“Until now we knew very little about the MX2 gene, but now we recognize both its potent anti-viral function and a key point of vulnerability in the life cycle of HIV,” Mike Malim, an infectious diseases professor at King’s College London, stated in a press release.
Laboratory Experiment
To better understand the body’s natural inhibitors and how to trigger them, scientists introduced the virus to two different human cell lines. Observing the effects, the researchers noted that in one cell line, the MX2 gene was ‘switched on’ (expressed), while in the other it remained ‘switched off” (silenced). Upon further investigation, they discovered that in the cells where the MX2 gene was expressed, the virus was not able to replicate and new viruses were not produced. Among those cells where that gene remained silent, though, the virus replicated and spread.
Considering their results, the researchers hypothesized possibilities for potential drug development in the future. “There are two possible routes — it may be possible to develop either a molecule that mimics the role of MX2 or a drug which activates the gene’s natural capabilities,” Malim stated in a press release. “It is important to continue to find new ways of mobilizing the body’s natural defense systems and this gene appears to be a key player in establishing viral control in people with HIV.”
Available Treatments
Currently, 31 antiretroviral drugs (ARVs) are used to treat HIV infection. Although these Food and Drug Administration (FDA)-approved drugs cannot ‘cure’ people, they do suppress the virus, sometimes to undetectable levels, and so allow an infected person to lead a healthier life. It is important to note ARVs, which must be taken continuously to provide benefit, do not eliminate HIV from the body, and infected people can still transmit the virus.
A recent study conducted in the UK suggests that patients with HIV may achieve life spans close to normal given certain conditions: adherence to antiretroviral therapy, maintenance of low viral loads and of CD4 counts above 350, and avoidance of injected drug use as well as co-infection with viral hepatitis. (CD4 cells, often called T-cells, send signals to activate the body’s immune response when they detect viruses or bacteria.) The results were derived from a total of 17,021 patients who started antiretroviral therapy (ART) in the years between 2000 and 2008. Of these patients, 708 or 4.2 percent died, while 3,956 or nearly a quarter of the total dropped out of the study.
A crucial issue among HIV/AIDS patients is adherence to their drug regimens. The difficulty of consistently taking several drugs or even one drug each and every day and the unpleasantness of side effects, such as nausea and vomiting, often cause patients to interrupt their schedule. When that happens, HIV may create more variations of itself, including strains that are resistant to the antiretroviral drugs taken by the patient. In general, half to three-quarters of all patients strictly adhere to their medication when it is prescribed over a long period of time. Nonadherence to ART, in particular, has been estimated at approximately 70 percent.
Source: Goujon C, Moncorge O, Malim MH, et al. Human MX2 is an interferon-induced post-entry inhibitor of HIV-1 infection. Nature. 2013.
May M, Gompels M, Sabin C. Life expectancy of HIV-1-positive individuals approaches normal conditional on response to antiretroviral therapy: UK Collaborative HIV Cohort Study. Journal of the International AIDS Society. 2012.



























