Swedish Doctors Perform 9 Uterus Transplants: Pregnancy Possible For Womb Recipients, But At What Costs?
After two failed attempts in Turkey and Saudi Arabia, the first successful uterus transplants are now expected to make the far leap to pregnancy, as Swedish doctors have introduced the organs into nine women who were born without wombs or have had it removed. Now, the women will attempt to give birth to their own children — a hallmark of the transplant that would become the first of its kind.
While limb transplants and the introduction of critical organs have been used with success for decades, uterus transplants are largely an unexplored frontier, or at least an unsuccessfully explored one. And despite the apparent success of giving a woman the chance to give birth, naturally, to her own child, some experts denounce the practice, claiming the quick-timed transplant and subsequent removal provides far more practical health risks than psychological benefits.
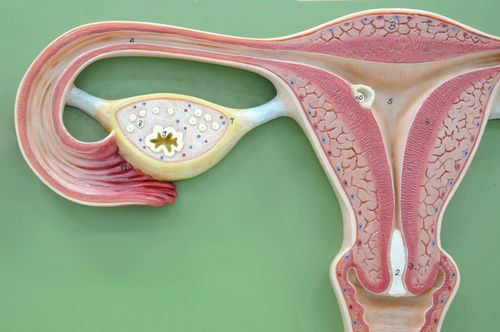
The women comprising the study are all in their thirties and either had their uteri removed, because of a related health concern, or were born without one — a condition known as Müllerian agenesis. The condition is also known as Mayer-Rokitansky-Küster-Hauser syndrome (MRKH), and with the exception of a missing uterus, women with the syndrome still ovulate and maintain proper hormonal balance. The foremost downside, of course, is that women with MRKH are unable to carry a pregnancy. They must rely on surrogacy or in vitro fertilization (IVF). But Swedish doctors now hope the transplantation procedure will alleviate that burden.
“This is a new kind of surgery,” Dr. Mats Brannstrom, study leader and chair of the obstetrics and gynecology department at the University of Gothenburg, told The Associated Press. “We have no textbook to look at.”
Previous attempts at transplanting wombs resulted in the patients’ bodies failing to “take,” or accept, the new organs, forcing doctors to remove them. But so far, many of the women in Brannstrom’s study have already had their periods six weeks after the transplant. One woman suffered an infection from the new womb, and a few others faced brief bouts of rejection, but all left the hospital within a few days, the AP reported.
The Cost-Benefit Analysis Of Uterus Transplants
Ultimately, the doctors hope each woman is able to give birth to her own child. They’ve allowed a maximum of two pregnancies before they remove the temporary womb, as the immunosuppressive anti-rejection medicine significantly increases a woman’s risk for high blood pressure, swelling, diabetes, and both uterine and cervical cancer. But these risks worry doctors who don’t see the act of delivering one’s own child as sufficient motivation for a woman to expose herself to such risks.
Dr. Kenneth F. Trofatter argues in an editorial for Healthline that the procedure carries no direct benefit for a female patient. “Indeed, the risks involved far outweigh any purported psychological benefits to women who were born without, or have prematurely lost, their uteri,” he explained. “The practitioners who will do this procedure will ‘be the first’ (and for that will obtain some degree of fame, or notoriety) but there is likely to be no major contribution to medical knowledge or technology that will come out of this procedure either.”
The women involved in Brannstrom’s study can’t get pregnant naturally, as the transplanted uteri aren’t connected to the women’s fallopian tubes. Prior to the study, researchers preserved the women’s eggs to be fertilized, and the resulting embryos will be transferred into the wombs to develop. Trofatter argues this process is unnecessarily complicated, based more on foolhardy pride rather than smart medical science.
“To be the first woman with a transplanted uterus to take this chance on a baby is, in my opinion, a selfish and foolish proposition,” he wrote.
Among the other concerns is whether a live donor is preferable to a deceased one. In the prior Turkish studies, the donor was dead. And while one woman got pregnant, ultimately it failed in two months’ time. Beside the myriad risks of rejection — an ill-connected placenta may fail to adequately nourish the developing fetus, for instance — British researchers also view the practice of live donation for a non-lifesaving procedure as unethical.
In the meantime, Trofatter’s concerns are mostly ethnocentric. IVF and surrogacy may be legal in the United States, but in many countries abroad the techniques are still outlawed. The experimental procedure of uterus transplantation offers a hope, albeit a risky one, but a hope nonetheless, to the one out of every 4,500 women born without a uterus who still wishes to bear children. The primary obstacle is securing the procedure’s safety in bringing it to the mainstream.
“What remains to be seen,” Dr. Yacoub Khalaf, director of the Assisted Conception unit at Guy’s and St. Thomas’ hospital in London, told the AP, “is whether this is a viable option or if this is going to be confined to research and limited experimentation.”



























