5 Major Hospital-Acquired Infections That Cost The US $10B Each Year
A new study published online in JAMA Internal Medicine finds total annual costs for five major hospital-acquired infections to be $9.8 billion.
The study, headed up by Dr. Eyal Zimlichman of Brigham and Women's Hospital in Boston, aimed to more precisely estimate costs associated with the most significant health care-associated infections (HAIs). Figures from past studies, according to Reuters, showed the total expense of treating such infections ranging anywhere from $20 billion to $40 billion. “Better evaluation of the costs of these infections could help providers and payers to justify investing in prevention,” wrote the authors.
To more precisely estimate total costs, Zimlichman and his team conducted a systematic review of the literature from 1986 to the current year. After excluding studies performed outside the U.S., they identified 26 studies from which they might identify the true cost associated with treating the five most common infections among hospitalized patients.
What did they find?
On an individual basis, central line-associated bloodstream infections were found to be the most costly at $45,814 per case. This was followed by ventilator-associated pneumonia at $40,144, surgical site infections at $20,785, Clostridium difficile infection at $11,285, and catheter-associated urinary tract infections at $896 per case. Total annual costs for these five major infections added up to just under $10 billion, with surgical site infections the largest of these expenses at just over one-third of total costs. Ventilator-associated pneumonia contributed nearly the same amount to the bottom line (31.6 percent), with central line–associated bloodstream infections logged at 18.9 percent, C. difficile infections 15.4 percent, and catheter-associated urinary tract infections less than one percent.
Preventable Infections
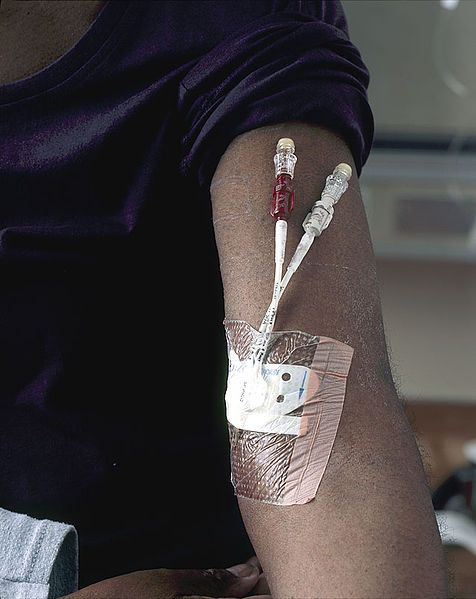
A central line catheter, also known as a central venous catheter, is a tube that is surgically placed in a large vein in the neck, chest, groin, or arm to give fluids, blood, or medications. When germs (usually bacteria or viruses) enter the bloodstream through the central line, this may cause a central line-associated bloodstream infection (CLABSI).
C. difficile, which is linked to 14,000 American deaths each year, causes diarrhea and those most at risk are people who take antibiotics. Older adults are among those most at risk. Generally, C. difficile is picked up from contaminated surfaces or spread from a healthcare provider’s hands.
A surgical site infection is an infection that occurs in the part of the body where the surgery took place. Many such infections are superficial and involve only the skin. Other surgical site infections can involve tissues under the skin, organs, or implanted material — these may be extremely serious.
Between 15 and 20 percent of all hospitalized patients receive urinary catheters during their hospital stay. A urinary tract infection (UTI) would be any infection in any part of the urinary system, including urethra, bladder, ureters, and kidney.
Finally, ventilator-associated pneumonia develops in the lungs of a person who is on a ventilator, a machine used to help a patient breathe. An infection may occur if germs enter through the tube and get into the patient’s lungs.
According to the U.S. Centers for Disease Control and Prevention, about one in every 20 hospitalized patients contracts an HAI. Although a threat to patient safety, HAIs can be prevented through caution and meticulous behavior, such as always "making sure a patient's skin is cleaned properly and that he or she is being prescribed the right dose of antibiotics," Reuters reported. For more information on prevention of HAI, please go here.
Source: Zimlichman E, Henderson D, Tamir O, et al. Health Care–Associated InfectionsA Meta-analysis of Costs and Financial Impact on the US Health Care System JAMA Internal Medicine. 2013.



























