Adult Stem Cells Manipulated To Mimic Embryonic Cells, Opening Door For Simpler Organ Growth
When the first human trial of embryonic stem cells hit the medical science landscape in 2009, the technology ruffled more than a few feathers. Pro-life advocates argued the procedure destroyed human life. Since then, science’s chief hurdle has been bypassing this concern, and according to a recent study, it have reached its destination.
It should be stated up front: Scientists are still operating in animal models. Indeed, ethics are still a worry. But for the time being, researchers at the University College London are confident their breakthroughs will lead to human trials one day. Their procedure involves converting adult stem cells, otherwise known as iPS cells, into embryonic cells by subjecting the cells to incredibly stressful, near-death states. Known as Stimulus-Triggered Acquisition of Pluripotency, or STAP, cells, the hybrid creations may offer scientists a cheaper, simpler route to the coveted prospect of artificially grown organs.
If the transition to humans is successful, “this could be the game changer that ultimately makes a wide range of cell therapies available using the patient's own cells as starting material — the age of personalized medicine would have finally arrived," Chris Mason, chair of regenerative medicine bioprocessing at University College London, who was not involved with the study, told Reuters.
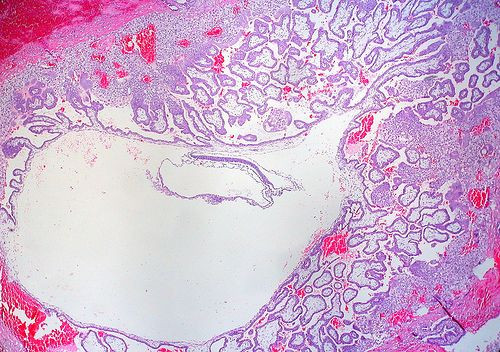
To conduct their study, the team took healthy adult stem cells from subjects’ skin and blood and put them under intense stress, to the point where they almost died. This included oxygen deprivation, trauma, and acidic environments. The latter of these, an acid wash, essentially bathed the cells in a high pH solution for approximately half an hour. Amazingly, after several days the cells had not only survived and replicated but had recovered by reverting back to an embryonic-like state.
Up next for the team is figuring out which of these mechanisms does the best job of catalyzing this conversion. Researchers working on the project included members from University College London, the RIKEN Center for Developmental Biology in Japan, Brigham and Women's Hospital, and Harvard Medical School.
"If we can work out the mechanisms by which differentiation states are maintained and lost, it could open up a wide range of possibilities for new research and applications using living cells," Haruko Obokata, who lead the work at RIKEN, told Reuters.
Stem cells are widely described as the body’s master cells. Like malleable heaps of clay, they’re capable of taking many shapes and fulfilling a range of designs. Through experimental trials, for instance, scientists have successfully designed a functioning liver and beating heart muscle tissue. These models may prove useful, experts speculate, in testing drug therapies without human intervention.
As for the latest research, it remains to be seen whether transferring the benefits of animal-supplied stem cells into humans is viable. Dusko Ilic, a reader in stem cell science at Kings College London, for one, said that he wouldn’t be surprised if this could result in a stem cell biology revolution “within the calendar year.” But others have less faith in the process’ expediency, claiming the actual migration from animal models to human subjects first needs a great deal of experimental unpacking.
"But the really intriguing thing to discover,” said Robin Lovell-Badge, a stem cell expert at Britain's National Institute for Medical Research, to Reuters, “will be the mechanism underlying how a low pH shock triggers reprogramming. And why does it not happen when we eat lemon or vinegar, or drink cola?"
Source: Obokata H, Wakayama T, Sasai Y. Stimulus-triggered fate conversion of somatic cells into pluripotency. Nature. 2014.



























