Woman Undergoes First Uterus Transplant In US; When Parenting A Biological Child Is The Only Option

Cleveland Clinic performed the nation’s first uterus transplant Feb. 24 during a nine-hour surgery on a 26-year-old woman with uterine factor infertility (UFI). The patient is reported to be in stable condition following the experimental procedure, which made use of a womb from a deceased organ donor. Around 5 percent of women worldwide have UFI, an irreversible condition most often caused by birth defects or medical treatments requiring removal of the womb.
A uterus transplant, which has been successfully performed in Sweden, offers infertile women the rare chance to carry a pregnancy. Why would a woman choose this instead of finding another pathway to pregnancy? After all, the surgery is complex, demanding, and risky.
The Process
Still in clinical trials, the surgery begins with an extensive evaluation. Teams of doctors, surgeons, psychologists, social workers, and bioethicists will sit down and talk with each possible candidate to determine who is “fit” for this experimental procedure. Once a woman is selected, extensive preparations begin. Because the eventual, hoped-for pregnancy must necessarily be in vitro (natural conception is not possible with a transplanted womb), a candidate will first have her eggs harvested. In a lab, her doctor will fertilize them with sperm and then select embryos for freezing, according to the Clevaland Clinic.
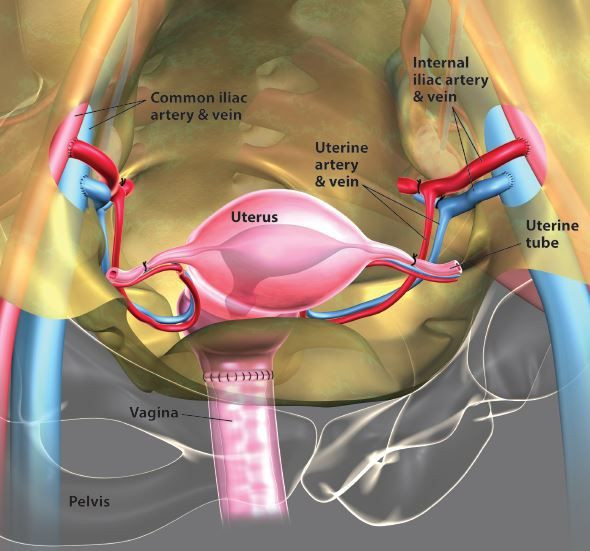
At this point, the actual transplant will occur. To prepare, the patient will take anti-rejection drugs, common to all transplant surgeries, while a healthy donor, between the ages of 18 and 40, is found. The donor’s uterus will be removed along with its blood supply and then transplanted into the woman’s pelvis. This time-consuming and difficult process includes connecting a donor’s blood vessels to the woman’s own.

Now, recovery begins. A few months after the transplant, the woman should start having periods and, 12 months later, her uterus should be fully healed. Here, her embryos are thawed and implanted, in turn, until one becomes a viable pregnancy. Continuing with her anti-rejection drugs, the woman’s pregnancy will be closely monitored by her doctors, who will perform monthly cervical biopsies to check for organ rejection. When the pregnancy comes to term, the baby will be delivered via C-section.
Finally, because they might cause her long-term physiological damage, the mother will stop taking anti-rejection drugs once she has decided she will have no more children. At that time, the womb will either be rejected or surgically removed, the clinic reports.
Risks
Undergoing egg-harvesting procedures and surgeries are risky, yet additional dangers exist; prior to a first-time Swedish victory, two separate medical teams failed in their attempts to transplant a womb. In one case, the uterus became diseased and had to be removed after three months. Another case resulted in miscarriages. Dr. Mats Brannstrom, the surgeon who led the first successful transplant on a woman born without a uterus, explains his extensive testing of the procedure in this video.
Importantly, he also notes the 15,000 live births among women who have had other types of organ transplants. Anyone who has received a donor organ continues to take anti-rejection drugs, which essentially suppress the immune system. He says, so far, the indications are these drugs do not lead to an increased risk of congenital malformations. Additionally, he found normal growth through adulthood for rat offspring produced as a result of a womb transplant.
However, one study of 62 pregnancies among women with transplanted organs reveals successful pregnancy outcomes, but higher than usual complication rates. Other studies find a higher risk of prematurity and pre-eclampsia in women taking anti-rejection drugs, however the rates were similarly high among this group of women before they began taking the drugs. Obviously, a pregnancy following a womb transplant is no easy path to walk, so why would a woman choose it?
A Biological Child
According to Dr. Susan Newman writing for Psychology Today, adoption is increasingly “snarled, discouraging, and costly” and that's true whether you adopt in the U.S. or internationally. Only 2 percent of American families adopt, quite possibly because there are too few newborns for the number of people hoping to raise them. Many would-be parents experience the heartbreak of winding up in a delivery room only to witness the birth mother changing her mind once seeing her baby.
Some people may be disqualified from adopting due to age, while others, including cancer survivors, may be excluded due to health reasons. Though some families turn to the welfare system, others are deterred once they learn most of the available children are over the age of three.
“I can attest to the fact that in that short lifetime, children in foster care will probably have been subject to considerable emotional and/or physical deprivation and/or abuse that leave scars and behavioral problems,” wrote Newman. As she notes, not all parents are financially or emotionally equipped to help a child past a rough early start.
Families who prefer to work with a surrogate instead of adopting are also confronted with a host of issues; unexpected emotional and legal issues often arise when another woman becomes involved in the process of birth.
While it is natural to want your own natural child first, it is not only the desire for a genetically-related baby that would drive infertile women to attempt a method, even an experimental technique, rather than to adopt. This ground-breaking uterus transplant brings hope to many infertile women wishing to become mothers.



























