Antibiotics: Superbug Threat Leads Doctors To Advise A Full Course Of Treatment
Discovered in the 1940s, antibiotics are powerful drugs that kill bacterial infections, including tuberculosis, strep throat, and urinary tract infections. Though highly effective for many infections, these medicines are powerless in the face of viruses and the many illnesses they cause, including flu and the common cold. Handing over a prescription for antibiotics, many doctors will caution their patients to take all of the medicine even after you feel better — “do not stop until all the pills are gone.”
Why the stern words attached to antibiotics?
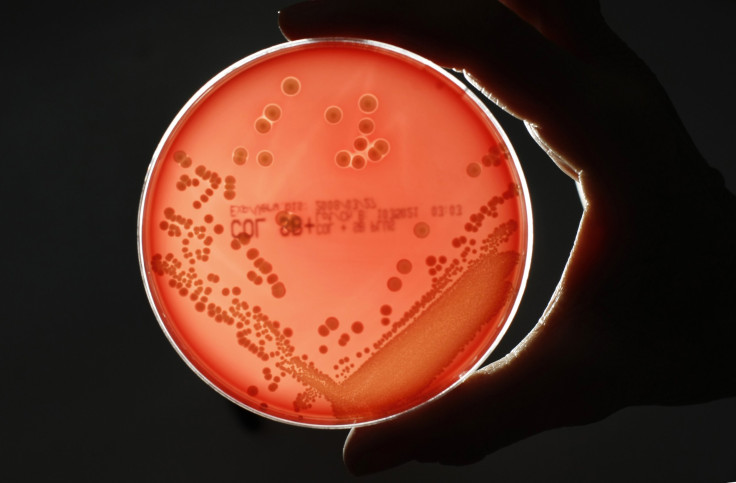
Bacteria are single-celled microorganisms. Your body is host to many bacteria, which live inside your digestive tract, on your skin, in both your mouth and genitals. Surprisingly, the bacterial cells in your body outnumber human cells by 10 to one. Many of these microorganisms, especially those in your gut, provide much-needed assistance with essential biological processes, such as breaking down your food.
Bacteria, then, are your friends for the most part… even if sometimes an enemy bug invades and makes you sick. When an antibiotic is prescribed, the intention is to kill only the bad microorganisms causing your illness while leaving the beneficial bacteria intact.
Unfortunately, the drug will kill only some, but not all, of the bad bacteria. Just as other genetic life forms mutate over time, the bad bacteria that manage to survive may modify their DNA in order to become stronger than the medicine, unable to be killed — this is "drug-resistance." With each dose of antibiotics, the more likely some of the surviving bacteria will become drug-resistant. Commonly, these resistant microorganisms are referred to as "superbugs."
The microscopic picture is even more complex. Whenever you take an antibiotic, you also kill off some of the beneficial bacteria living inside you. A slight void will be created, allowing any resistant bacteria to rush in, multiply, and transfer their drug resistance to other bacteria. For this reason, over-use of antibiotics — using these drugs when the body will heal on its own or using these drugs for viral infections that they do not treat — contributes to the problem of superbugs.
In big picture terms, what this means for you is greater danger. If the bacteria inside you become drug resistant, you could develop a recurring infection, which will be more difficult to treat — the same drug will not work and a new antibiotic will be prescribed. Each year, antibiotic-resistant infections sicken about two million Americans, the CDC reports, while killing 23,000. Increasingly, resistant infections will occur anywhere, though commonly they happen in hospitals, nursing homes, and similar facilities.

When a doctor advises you to take all your medicine, then, the hope is all the bad bacteria in your system will be destroyed with none surviving and becoming resistant. Yet the issue is even more complicated and certainly more contentious. As this New York Times article suggests, a "standard" course of antibiotic treatment is anything but "standard" since different doctors will prescribe a different duration of treatment. Meanwhile, this Discover article reports newer data from multiple studies lend support to the idea that lower doses are better and less likely to lead to resistant bacteria.
Though Medical Daily would never suggest you mindlessly obey your doctors, you are paying for their educated advice about what dosage is best, so you might want to discuss the issue and get a better understanding of their thinking.
Whether right or wrong, doctors issue their dire warnings for you to take all your pills as an attempt to prevent the emergence of too-strong bacteria. While most people find it easy to understand that over-using these drugs leads to resistant bacteria, the much more difficult concept is that under-treatment also may result in deadly superbugs. Sadly, whenever you improperly use strong medicines, you not only become a danger to yourself but also to your community and the wider world.



























