Australia’s Free HPV Vaccine Program Reduced Genital Warts Cases By 61%; Also Reduces Their Risk Of Cervical Cancer
Since the introduction of the National Human Papillomavirus (HPV) Vaccination Program in Australia in 2007, the number of genital warts cases has gone down by 61 percent, according to a new study from University of Sydney.
The study, based on medical reports from general practitioners, found that there was a gradual but significant decrease in the number of genital warts cases in women aged 15 to 27 since the program began. The findings were published in the journal PLOS ONE.
"The results show that the program has been a widespread success," said lead author Christopher Harrison, of the University of Sydney, in a press release. The number of genital wart cases fells from 4.33 per 1,000 people pre-program (2002 to 2006) to 1.67 per 1,000 people in the post-program period (2008 to 2012).
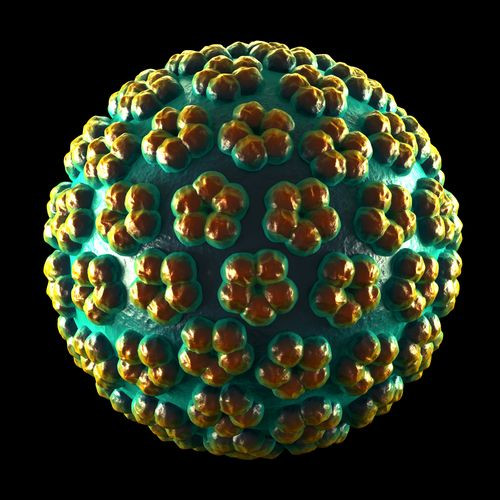
HPV is a common sexually transmitted disease. It is estimated that all sexually active men and women at some point in their lives get infected by it, and it's generally transmitted through sexual contact with an infected person. There are different strains of HPV, and while most go away without causing any serious harm, those that do persist can cause genital warts and cancer.
Carriers of the virus may not even be aware of it since symptoms don’t usually appear. The best way for a person to lower their chances of getting infected by HPV is to get vaccinated. Boys and girls are generally given the vaccine before they hit puberty. Australia was among the first countries to provide the HPV vaccine for free in schools as part of the national program. The vaccine protects against two major strains that cause genital warts (HPV 6 and 11) and two major strains that cause cervical cancer (HPV 16 and 18). This study is the first to look at the impact of the immunization program.
"We looked at women potentially covered by the vaccination program (15 to 27 years), and the data showed a 61 percent decrease in the management rate of genital warts in the four years after the program started, compared with the four years before the program,” Harrison said. "For all other age-sex groups (who were not covered by the program) there was no significant change in the management rate of genital warts between the pre-program and post-program periods.”
The study also found that there was no significant decrease in other sexually transmitted disease cases during the time period, which further proves that the reduction in genital warts was due to the vaccination program and not because of a change in the sexual behavior of women. “The program has proved to be a great success and of huge benefit to the sexual health of Australia, and has clearly proven to be very worthwhile," Harrison concluded.
Source: Harrison C, et al. PLOS ONE. 2014.



























