Bad Cholesterol Targeted In New Protein-Busting Research
Researchers have successfully targeted a protein that interferes with the liver's ability to remove cholesterol from the bloodstream - in mice.
Scientists at the University of Michigan affilated with the Howard Hughes Medical Institute disrupted the action of the SEC24A gene, trapping the nefarious protein away from receptors responsible for removing clear plasma cholesterol from the blood without otherwise affecting the health of the mice.
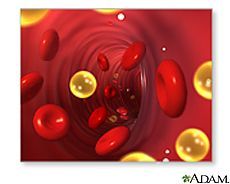
In fact, researchers led by Dr. David Ginsburg found that mice with the inactive gene developed normally, with the only perceptible difference a 45 percent reduction in plasma cholesterol levels. With the "proprotein convertase subtilisin/kexin 9" protein missing in action, liver cells were better able to remove low-density lipoprotein (LDL), or "bad cholesterol," from the bloodstream. The secretory protein normally disrupts the LDL receptors of liver cells.
"Inhibiting SEC24A or PCSK9 may be an alternative to statins, and could work together with statins to produce even greater effects," said Dr. Xiao-Wei Chen, lead author of the research. "Also, they might be effective on patients who are resistant to or intolerant of statins."
Preliminary research into human therapies have shown that disrupting the protein lowers bad cholesterol significantly and even works with statins such as Lipitor to further reduce levels. Experts say the study suggests researchers might next seek to block the transport mechanism - rather than the protein itself. The study also explains the transport mechanism for the protein, by which liver vesicles transport the disrupter within the cell. Ginsburg's research team focused specifically on a type of vesicle packaged by "Coat Protein Complex II," which regulates the metabolism of cholesterol among other functions.
Such vesicles act as vehicles for the protein and others.
"Without SEC24A, much of the [protein] couldn't make its way out of the cells to destroy the LDL [receptors], which then clears cholesterol from the blood," Dr. Chen said.
With the protein effectively disabled, at least much of the time, the liver was able to rid the body of cholesterol that would otherwise clog the arteries, increasing the risk of stroke and heart disease.
Ginsburg said he had "no reason at this point to expect that this strategy will be any better than anti-PCSK9 therapy for treating high cholesterol" but emphasized that an alternative approach would give science more options to pick and choose which drugs might work best in therapy.
The study was reported in the journal eLIFE.



























