Scientists Recreate Beating Heart, Functional Liver With Microchips In Hopes Of Improving Drug Testing
Animal testing for organ transplants may soon be a problem of the past thanks to recent advancements in regenerative medicine and tissue engineering. A research team from the University of Toronto have designed a “person-on-a-chip”— a 3D microchip lined with human cells that mimics the complex organ systems within the body. The study, published in Nature Materials, gives scientists new opportunities to grow human cells outside the body and test for potentially dangerous drug side effects.
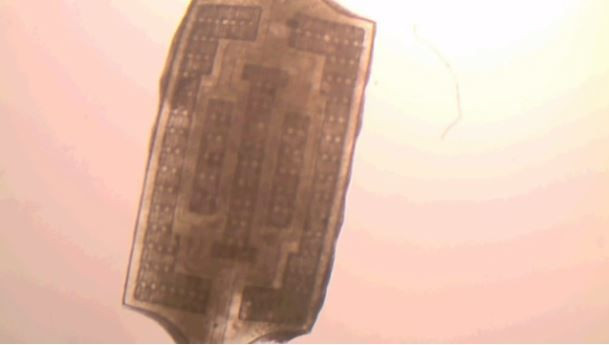
Called the AngioChip, it’s a “fully three-dimensional structure complete with internal blood vessels," said the study’s lead author Milica Radisic, a professor at the Institute of Biomaterials & Biomedical Engineering at the University of Toronto, in a press release. "It behaves just like vasculature, and around it there is a lattice for other cells to attach and grow.”
Researchers built the AngioChip out of a clear, flexible polymer about the size of a computer memory stick. Within the chip are tiny scaffolds about as wide as a human hair, which create hollow channels that can be lined with living human cells. This effectively creates artificial blood vessels, which can be stacked on top of other chips, bonded, and made into a 3D synthetic vascular system.
When the structure is complete, researchers bathe it in a liquid of live cells, which attach to the inside and outside of the scaffolds and begin to grow as if they are inside the body. After about four weeks, the team saw heart cells grow substantially on the microchips, and begin to behave like an actual organ. Once it became fully functional, the researchers watched as its flexible polymer scaffold contracted and expanded in a regular rhythm, just like a normal heartbeat.
What sets the AngipChip apart from other synthetic organs is that it can be built to include multiple organs on one chip. The researchers did this with liver cells, which they found could then produce urea, the main compound in urine, as well as metabolize drugs. When this chip was connected to the heart chip, the researchers could watch not only how certain drugs affect each organ but also how they affect both organs at the same time.
"In the last few years, it has become possible to order cultures of human cells for testing, but they're grown on a plate, a two-dimensional environment," Radisic said. "They don't capture all the functional hallmarks of a real heart muscle, for example.”
The AngioChip has the potential to change the way humans test drugs by creating realistic models at a fraction of the cost. On average, it takes roughly $5 billion to develop a drug, and 60 percent of those funds go to research and development of live organ tissue testing. Microchip models would eliminate this expensive approach, and cut the time it takes to bring a new drug to the market. The microchips would also reduce the need for animal testing, which is used to determine any drug side effects.
”It really is multifunctional, and solves many problems in the tissue engineering space,” Radisic said. “It’s truly next-generation.”
Source: Radisic M and Zhang B, et al. Nature Materials. 2016.



























