Bone-Marrow Transplant Halts Rett Syndrome in Mice, Prolongs Life and Reverses Symptoms
Bone marrow transplants that boost a type of brain immune cells could potentially be used to treat Rett syndrome, a severe and incurable autism spectrum disorder that affects about one in every 10,000 girls, by improving the debilitating symptoms associated with the disease and significantly extending patient lifespan.
Researchers were able to significantly improve symptoms, extend lifespan substantially beyond what was expected, increase body size and reduce tremors by transplanting bone marrow in in a mouse model of the disease.
The findings, published on March 18 in the journal Nature, suggest that boosting the brain’s immune cells called microglia, which are defective in Rhett syndrome, via bone-marrow transplants or by other means could help treat the disease.
“If we show the immune system is playing a very important role in Rett patients and we could replace it in a safe way, we may develop some feasible therapies in the future,” one of the lead researchers Jonathan Kipnis, a neuroscientist at the University of Virginia School of Medicine in Charlottesville, told Nature.
Rett Syndrome is the most physically disabling of the autism spectrum disorders, and it is caused by random mutations in the gene MECP2 on the X chromosomes, and because females are born with two X chromosomes, the other X is usually normal enough for the child to survive past birth. However, males born with the defective gene usually results in stillbirths, miscarriages or very early death.
Symptoms usually begin between 6 to 18 months of age, when children lose acquired language skills and functional hand use, and movement generally deteriorates as other symptoms start to appear. Other symptoms are abnormal breathing, Parkinson-like tremors, severe anxiety, seizures, digestive and circulatory problems and a range of autonomic nervous system and orthopedic abnormalities, and while most children survive to adulthood, most are wheelchair-bound and require lifelong care.
Researchers said that the MECP2 protein is responsible for the activity of many other genes, but they are still unsure as to why its mutation causes Rett syndrome.
Investigators used radiation to wipe out the immune systems of mice affected by a gene mutation equivalent to MECP2, and injected bone marrow from genetically normal mice into the mutated mice and found that the procedure gave the mutant mice a new immune system that was genetically normal.
Mutated mice that did not receive bone marrow injections got sick within weeks of birth, were underweight, had tremors, had irregular breathing, could barely move, and died within 8 to 10 weeks after birth.
While the untreated mice dead with many debilitating symptoms, the mice treated at 4 weeks old had dramatically reduced symptoms, and the oldest of them lived almost a year.
"This seems to stop the disease in its tracks," the other lead researcher Noël Derecki told Nature.
Researchers found that by restoring the MECP2 gene’s normal function in the mice neurons, which express more MECP2 than any other cell in the brain, they successfully reversed some of the disease’s symptoms.
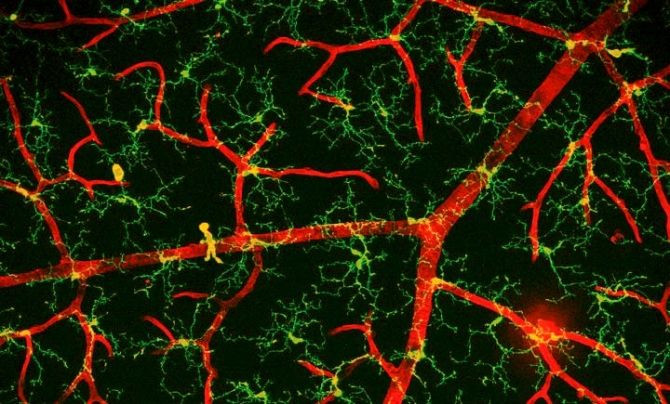
Although investigators are still unsure as too why symptoms of the disease appeared to stop after the marrow transplants, they suspect that by introducing genetically normal microglia, which act as the first and main type of the active immune system in the central nervous system by scavenging and swallowing any damaged neurons, plaques, and infectious agents in the nervous system, was the main reason for the improvements in symptoms.
Researchers explained that when they injected transplanted mice with a rug that prevents microglia from absorbing the brain’s cellular garbage, the benefits of the transplant seemed to vanish.
"Our work shows that if you can make their environment healthier, even sick neurons can function better," Kipnis told Nature.
While scientists from the latest research caution that more additional research is required to assess the treatment potential, they believe that their findings offer an important glimpse into the biology of the disease, and that bone marrow transplants may help those with Rett syndrome.
The said that gene therapy to fix MECP2 mutations is unavailable and the idea is far beyond technology, but by improving the brain environment by adding more defense microglia cells, there may be a way to diminish some aspects of the disease.
While, bone marrow transplants are currently performed on children with leukemia and other cancers, the high-risk procedure carries serious and sometimes even fatal side effects.
Gail Mandel, a neurobiologist at the Vollum Institute in Portland, Oregon, said while the findings are “fascinating,” it’s still too early to think about human therapies based on the evidence presented in the latest research. Future research needs to determine how the microglia restore neural function, and for how long, she said in a statement.
Other researchers question whether the same findings would be found in humans as they were found in mice.
“A question that arises, of course, is whether replacing faulty immune cells with healthy microglia through bone marrow transplant would arrest or ameliorate already existing symptoms in humans. We do know of a case in which a girl with Rett Syndrome who was treated for leukemia gained considerable communication skills after a bone marrow transplant, and was able to converse with her mother for the first time in their lives. RSRT is in the process of exploring bone marrow transplant as a treatment modality, with full awareness of the serious nature of such a trial. In research, we are risk-takers. In clinical application, we are conservative and will be examining this carefully as more information emerges," Monica Coenraads, Executive Director of the Rett Syndrome Research Trust, said in a statement.
Published by Medicaldaily.com



























