Brain Scans Show OCD And Schizophrenia Share Common Loss Of Gray Matter
Many people question the fact that psychiatrists often diagnose mental illness based on symptoms alone, even when no biological basis for a particular mental disorder can be found — where’s the proof? they ask. Now, a new study from Stanford not only collects some hard evidence but also offers unexpected insight into potential causes or outcomes of psychiatric conditions. Analyzing whole-brain images from nearly 16,000 people, researchers identified a similar pattern — a loss of gray matter in three brain structures — across a spectrum of disorders commonly believed to be distinct.
Neuroimaging has impacted the field of psychiatry tremendously; however, most brain scan studies simply analyze brain structure and function in healthy volunteers and compare this to the same analysis of patients with a single, specific diagnosis. Though a 2013 genetic analysis showed several categories of mental illness shared a genetic origin, rarely, if ever, do neuroscientists look at a range of mental disorders and try to glean information concerning all of them at once. For the current study, then, the research team decided to focus on answering a simple question: Does a common biological basis for mental illness exist?
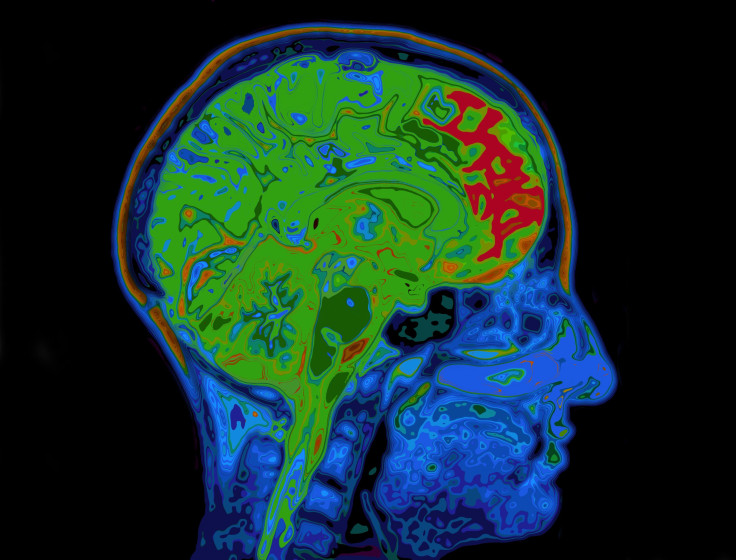
To answer that question, Dr. Amit Etkin, an assistant professor of psychiatry and behavioral sciences at Stanford, and his colleagues gathered data from 193 separate studies containing MRIs from 7,381 psychiatric patients. Each patient had been diagnosed with schizophrenia, bipolar disorder, major depression, addiction, obsessive-compulsive disorder, and/or a cluster of related anxiety disorders. Next, the researchers collected brain scans from 8,511 healthy volunteers and went to work analyzing and comparing the many images.
The team identified three separate brain structures, several centimeters apart from one another, where patients showed a decreased volume of gray matter in comparison to the healthy volunteers. Surprisingly, this loss of gray-matter was similar across patients with different psychiatric conditions, the researchers found. The affected structures — the left and right anterior insula and the dorsal anterior cingulate — are known to be parts of a larger brain network associated with higher-level executive functions such as concentrating in the face of distractions, multitasking or task-switching, planning and decision-making, and inhibition of counterproductive impulses.
“Secondary analyses also suggest that these findings are likely not due to medication effects,” wrote the authors.

Alarm Bells
The patients diagnosed with depression also showed gray matter loss in the hippocampus (memory) and amygdala (emotion), while those diagnosed with schizophrenia had an increase in gray matter in the striatum, which coordinates motivation and body movement. In this case, antipsychotic medications may have caused this, Etkin said, and not progress of the disease itself.
Perhaps the most interesting implication of this research is the fact that the left and right anterior insula and the dorsal anterior cingulate function as “the alarm bell of the brain,” in Etkins words, who added in a release,“They work together, signaling to other brain regions when reality deviates from expectations — that something important and unpredicted has happened, or something important has failed to happen.” Considering some psychiatric patients are plagued by delusions and, in some cases, hallucinations, this lack of an "alarm bell" gives substance to theories that patients' brains have lost the ability to distinguish reality from fantasy.
Source: Goodkind M, Eickhoff SB, Oathes DJ, et al.Identification of a Common Neurobiological Substrate for Mental Illness. JAMA Psychiatry. 2015.



























