Cancer Breakthrough: New T-Cell Therapy Produces ‘Extraordinary’ Results In Terminal Blood Cancer Patients
A new cancer therapy that employs molecules from genetically altered mice to help patients’ immune systems better detect cancer and destroy it has been hailed as “extraordinary,” with efficacy rates normally considered to be “unprecedented in medicine.” If the results are confirmed, the technique could usher in a new era for cancer treatment, according to a report published by The Guardian.
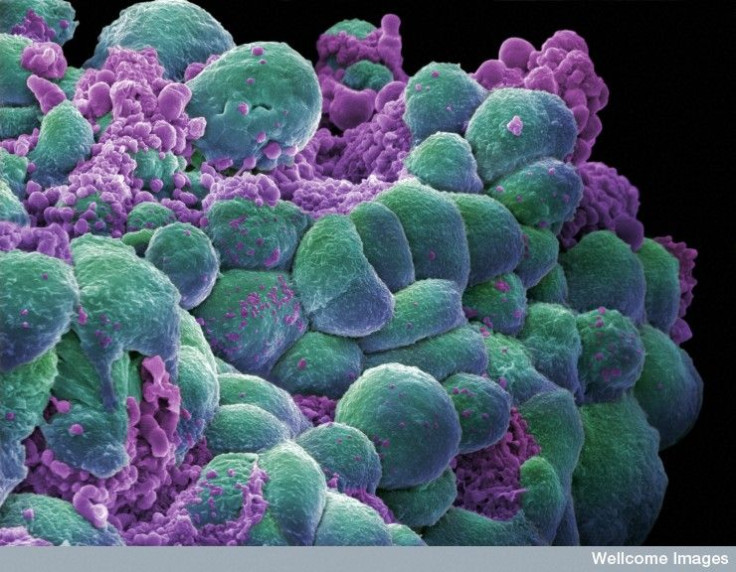
The body is naturally able to defend itself against disease and infection. Cancer cells, however, are capable of evading the body’s defenses by interfering with the immune system’s ability to recognize them as a threat, or by suppressing the immune system altogether. This helps the cancer cells to metastasize, or spread throughout the body, and eventually turn into life-threatening tumors. The new therapy counters this effect, helping the immune system recognize the danger.
The treatment first involves collecting T-cells from the bodies of blood cancer patients. These immune cells are responsible for both identifying pathogens and remembering returning pathogens to trigger a faster immune response. Doctors then tag the T cells with a “receptor” molecule derived from genetically altered mice, known as chimeric antigen receptor (CAR), which can attach to both T-cells and tumor cells. Once the tagged T-cells are reintroduced to the cancer patient’s body, they work to prevent cancer evasion from the immune system by helping T-cells target and destroy cancer cells. .
To date, the treatment has only been used on several dozen patients with various types of blood cancer. Although a paper reporting the research is still in review and unpublished, The Guardian reported that some results are already being shared with the public. One study on acute lymphoblastic leukemia, for example, found the treatment eliminated 94 percent of all symptoms. Patients with other types of blood cancer also left the trials with excellent outcomes; response rates were greater than 80 percent and more than half experienced complete remission.
In a recent speech at the annual meeting of the American Association for the Advancement of Science, lead author Dr. Stanley Riddell expressed optimism over the results. While further research is necessary, he said the current results are a “potential paradigm shift” for cancer treatment, Sky News reported. “This is unprecedented in medicine, to be honest, to get response rates in this range in these very advanced patients,” he said.
T-cells are an especially useful target for treatment because of how durable they are. They can live inside a patient's body for years following an initial transfusion, thus providing long-term protection. Yet, there are still risks to T-cell therapy. They’ve previously been associated with cytokine release syndrome, a condition that can lead to hypotension, neurotoxicity, or death from having too many T-cells in the body. Riddell says limiting the number of T-cells doctors reintroduce into patients’ bodies can help prevent this. “There are reasons to be optimistic, there are reasons to be pessimistic,” he said.
For now, the therapy works best on tumors found in blood and bone marrow. The eventual goal is to perfect the process so that it works for any patient, no matter the type of cancer they have, the Guardian reported.



























