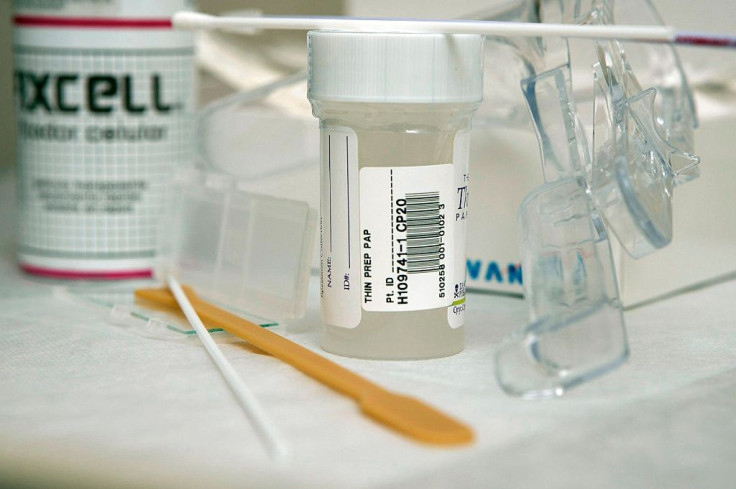
Chlamydia Testing Dropped Among Women When New Guidelines For Pap Smears Were Released
Do current pap smear guidelines lead to a drop in STD screening? In a new study from the University of Michigan (U-M), researchers are inclined to say yes.
In 2009, the national health test guidelines were amended to recommend women get pap smears every three to five years once they turned 21. Up until that point, women were only advised to get the test, which can detect and prevent cervical cancer, as early and often as they could. Health clinics believed this ambiguity factored into why they were ordering so many unnecessary follow-up tests.
Yet, when the 2009 guidelines were released, U-M researchers suspected they would lessen the chances women would opt-in for additional health tests, like STD screenings. Within their own family medicine clinics, researchers saw pap smears and chlamydia screenings were performed together 60 percent of the time. Chlamydia in particular is known to affect more young women than men, according to the Centers for Disease Control and Prevention, and women who have chlamydia are often asymptomatic.
To test their hypothesis, the researchers looked at tests given to sexually active women aged 16 to 21 ahead of the new guidelines — these women underwent their tests at one of U-M’s five family medicine clinics. Then, the researchers looked at tests given to women two years after the changes were made. Neither group of women had shown symptoms of chlamydia.
The researchers found women who got tested before the changes were 14 times more likely to get tested for chlamydia than those who were screened years later, even though U-M’s clinics reported their usual number of clinic visit by patients. What’s more is the likelihood of these tests being performed together had dramatically dropped to 10 percent.
The missing element seems to be the pelvic exam. An exam is necessary to test for cervical cancer, but it’s not necessary to test for chlamydia. As an alternative, women can test their urine for the STD. Dr. Allison Ursu, lead study author and lecturer in U-M’s Medical School Department of Family Medicine, said that “the clinical framework of the visit shifts when we’re not doing a pelvic exam, and the things we’re thinking about are different.”
Senior study author Dr. Mack Ruffin added: "Patients are very aware of pap tests and many still think they need one yearly. There's much less awareness of chlamydia screening. The takeaway from this study is that we have to find other opportunities to screen."
Source: Ursu A, Sen A, Ruffin M. Impact of Cervical Cancer Screening Guidelines on Screening for Chlamydia. The Annals of Family Medicine. 2015.
Published by Medicaldaily.com



























