Chlamydia Treatment Often Difficult Due To Pathogen's Resilience; Scientists Trace STD's Evolutionary Pattern
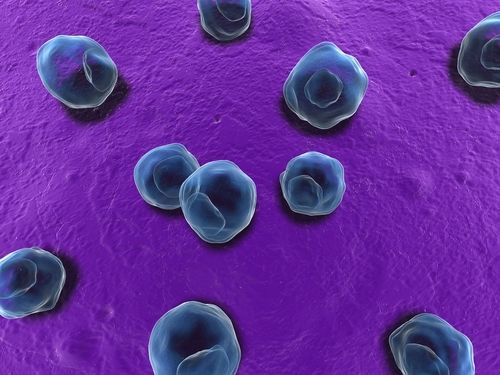
Anyone who has suffered from the sexually transmitted disease (STD) caused by the bacterium chlamydia would know how difficult it is to get it diagnosed and treated. It is the most widespread form of STD in the U.S. today, and experts agree that identifying the exact phenotype of the bacterium is a huge step toward developing therapeutics targeting it. After years of exploring the genetic evolution of the bacterium, researchers from the University of Vienna finally discovered the secret behind the pathogen’s resilience: recombinations.
The Centers for Disease Control and Prevention estimates that over four million Americans get affected by a species called Chlamydia trachomatis that causes STDs. Also, since more than half the people do not exhibit symptoms, they remain active spreaders. Women are especially vulnerable as the disease is known to cause infertility, life-threatening ectopic pregnancies, damage to sex organs, premature deliveries, and cervical cancer. It is also a major cause of blindness in poor countries, with more than 100 million people suffering from severe visual impairment due to infection by C. trachomatis.
For some years now, scientists have suspected that recombination factors play a key role in the genetic diversity of this bacterium — factors that may provide some biological advantages to it, such as pathogenicity, antigens, proteins, etc. To identify the exact factors, the research team sequenced four new strains, genetically related to the chlamydia strain and compared them with existing DNA data.
They found an extensive and robust shuffling of the genomic deck between chlamydia families — a factor that has contributed to the evolution of the pathogen and its ability to hoodwink host immune cells. They also identified genomic hotspots that seem to play a key role in adaptation and survival, with many having an unknown function. Specifically, these gene families were found to carry several protein factors gained from eukaryotic hosts.
The researchers further analyzed these proteins by performing cell-based assays and found that these proteins often interfere with the host’s defenses. The authors turn to the concept of the "birth-and-death" evolution to explain the genetic diversity of chlamydia. This hypothesis states that new genes are created by gene duplication, and some of these duplicated genes persist in the genome for a long time, whereas others are lost or deleted from the genome.
This type of evolution generally appears in highly conserved genes, so finding it in an obligate intracellular human pathogen was a bit surprising.
"One of the most surprising findings is that a similar mode of evolution has so far only been observed in fungi, plants, and animals." said lead researcher Matthias Horn in a press release.
But this discovery is a step forward in identifying how chlamydia persists in humans and to develop next-generation therapeutics targeting these genetic hotspots, say the researchers.
"Our study highlights the importance of taking advantage of the tremendous diversity of environmental microbes to improve our knowledge about the evolution of microbial pathogens," coauthor Domman said.
Source: Domman et al. Molecular Biology and Evolution. 2014.



























