If I have allergies, should I get the coronavirus vaccine? An expert answers this and other questions


Editor’s Note: With a coronavirus vaccination effort now underway, you might have questions about what this means for you and your family. If you do, send them to The Conversation, and we will find a physician or researcher to answer them. Here, Dr. Mona Hanna-Attisha, a public health pediatrician whose research exposed the Flint, Michigan, water crisis, answers questions about the vaccine and allergies, and when kids might be able to get the vaccine.
If I have allergies, should I still get the vaccine?
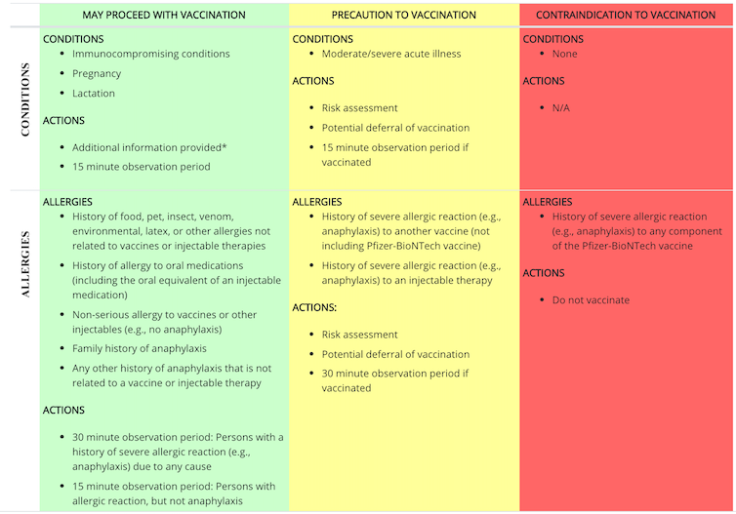
If you have a history of allergies to food, pets, insects or other things, the Centers for Disease Control and Prevention recommends that you proceed with vaccination, with an observation period. If you have a history of severe allergic reaction, or what is called anaphylaxis, to another vaccine or injectable therapy, your doctor can do a risk assessment, defer your vaccination, or proceed and then observe you after vaccination. The only reason to avoid vaccination is a severe allergic reaction to any component of the COVID-19 vaccine. The CDC has specific recommendations for post-vaccine observation.
As the vaccine goes out to a broader population, how will adverse events be tracked?
The CDC and Food and Drug Administration encourage the public to report possible adverse events to the Vaccine Adverse Event Reporting System, or VAERS. This national system collects these data to look for adverse events that are unexpected, appear to happen more often than expected or have unusual patterns of occurrence. Anyone who has experienced an adverse event should report it to the system.
Reporting an adverse event is a crucial step to ensuring safety and to help the CDC monitor the vaccines. Safety is a top priority, and scientists and public health officials need to know about adverse reactions.
An adverse event is different in most cases from a typical vaccine side effect. Vaccines may cause a side effect, such as soreness at the injection site or redness. Adverse events are more serious and can sometimes be life-threatening. If you are unsure whether you have experienced a side effect or adverse event, you can still report the event.
Participants are given a fact sheet when they are vaccinated. Health care providers who vaccinate people will be required to report to VAERS certain adverse events following vaccination. In addition, under the terms of the emergency use authorization, health care providers also must follow any revised safety reporting requirements that may arise.
The CDC is also implementing a new smartphone-based tool called v-safe to check in on people’s health after they receive a COVID-19 vaccine. When you receive your vaccine, you should also receive an information sheet telling you how to enroll in v-safe. If you enroll, you will receive regular text messages directing you to surveys where you can report any problems or adverse reactions you have after receiving a COVID-19 vaccine.
When might kids younger than 16 be vaccinated?
It is likely to be several months. The currently authorized Pfizer and soon-to-be-authorized Moderna vaccine are not applicable for children. More research and clinical trials need to be done to include younger children in COVID-19 vaccine trials.
According to the American Academy of Pediatrics, Pfizer has enrolled children down to age 12 and submitted a request for emergency use authorization for vaccination down to age 16. Moderna, whose vaccine is expected to receive emergency use authorization from the FDA any day, is about to start a similar study.
In the United Kingdom, AstraZeneca has approval to enroll children ages 5 to 12 in clinical trials, but the pharmaceutical company has not yet enrolled any children in trials in the U.S.
Mona Hanna-Attisha, Professor of Medicine, Michigan State University
This article is republished from The Conversation under a Creative Commons license. Read the original article.



























