Drug-Resistant Yeast Infection Spreading In US Hospitals; Fungus Linked To 4 Deaths

A new deadly infection has been hitting weakened people throughout the world, and scientists aren’t exactly sure how it is spreading or how to fight it.
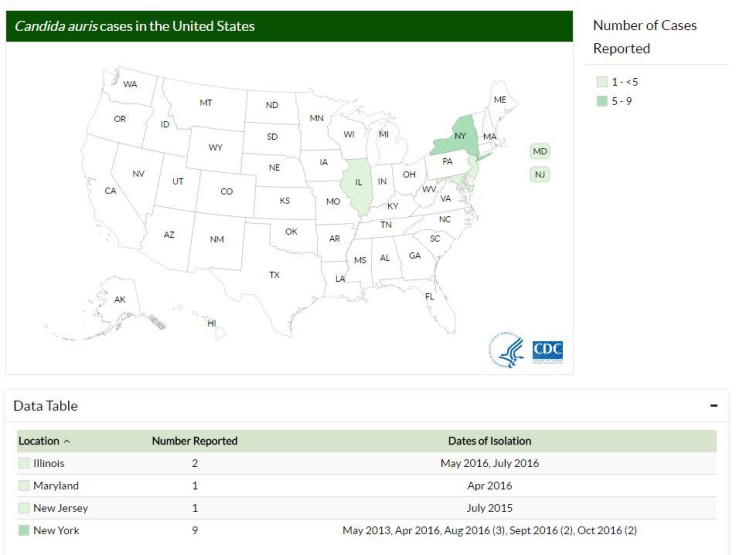
The Candida auris yeast superbug has killed four people in the U.S. in the last few years and sickened several more, according to a report from the Centers for Disease Control and Prevention. The yeast caused serious infections in their wounds and bloodstreams; most of the cases occurred this year and in New York State. Organisms and bacteria like MRSA cause deadly infections in hospitals and other health care facilities through contact with contaminated equipment or hands, but this yeast is different because C. auris is behaving differently from how fungi normally do — it is hard to detect and it doesn’t respond to antifungal medications. All four U.S. patients who died had the infection in their blood, while others had the infection in their blood, urine or ear.
“I am worried,” Tom Chiller, a physician who is chief of the CDC’s mycotic diseases branch, told National Geographic. “I think this is a real threat.”
The magazine notes that the yeast was first noted causing an infection in Japan in 2009, and it has since popped up in regions around the globe, sickening dozens of patients. The strains are in the same family but may have arisen separately, in different places at the same time. “In various locations, up to two-thirds of those who've been infected with this new fungus have died.” Making matters worse, while a couple of those infected in the United States spent time in the same health care facilities — but at different times — there is no link between any of the other cases “and none of the patients have anything in their recent past that would explain their infections.”
Those people, however, all had serious medical conditions, like cancer, for which they were receiving a lot of medication that could potentially weaken their immune systems, National Geographic explains. And on top of cycling between health care facilities, which can spread infection, “they're touched by lots of caregivers and connected to lots of equipment, both of which could spread the organism onto their skin or into their bodies.”
“We consider this a serious threat that we want to act on aggressively,” Chiller told the magazine. But without knowing its source or how to treat it, that means simply isolating patients and enforcing strict rules on cleanliness. Even before its new report was released the CDC has recommended those measures.
C. auris isn’t like other yeast infections that immediately come to mind. In a vaginal yeast infection, for example, yeast that lives naturally and safely in a woman’s body overpopulates, causing itching and burning, among other symptoms, the Mayo Clinic notes. In the mouth, that kind of infection is often called “thrush.”
There are other yeast infections in the body as well, such as those that can affect the blood, eyes, heart, brain or bones. The bloodstream yeast infection, in particular, is common in hospitals in weakened patients. The CDC says those break out when naturally occurring yeast on the skin or in the gastrointestinal tract slips into the patient’s blood, such as through an opening created with a catheter.
But in those cases, National Geographic points out, “People are the sources of their own infection.” With C. auris, however, “the source of the infection isn’t the person who got sick. It seems instead to be the hospital environment, including catheters, counters, and other surfaces. Also, this new yeast is causing outbreaks, which again is very unusual and has epidemiologists alarmed.”
Further reading: CDC report, “Investigation of the First Seven Reported Cases of Candida auris, a Globally Emerging Invasive, Multidrug-Resistant Fungus”
Published by Medicaldaily.com



























