The Effectiveness Of Birth Control, Plus 3 More Things We Recently Learned About Birth Control Methods
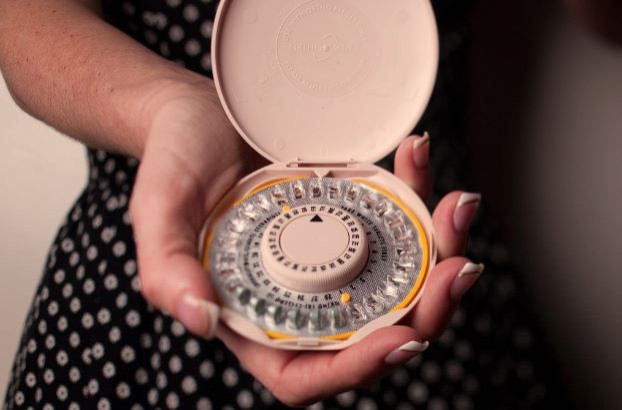
Birth control methods have been around for thousands of years. In ancient China, women drank lead and mercury to control their fertility, while women living in the Middle Ages in Europe were advised to wear amulets of herbs and broken cat bones — for real. The first oral contraception didn’t appear until 1960, and (thankfully) since then, birth control methods have only further improved.
There are so many forms of birth control available today that in 2012, the Planned Parenthood Federation of America (PPFA) calculated it provided birth control information and services to 2.1 million patients. Its services, PPFA added, helped prevent 516,000 unintended pregnancies; 217,000 abortions; as well as provide 500,000 life-saving breast exams and nearly 4.5 million tests and treatments for sexually transmitted diseases. That’s not to say unintended pregnancies and abortions are no longer a problem, or that every woman is using contraception, but it is to say society has come a long way from asking women to poison themselves with lead.
What are some of the more recent revelations we’ve had when it comes to birth control and women’s health?
Some Risks Are Common
The National Campaign to Prevent Teen and Unplanned Pregnancy and Cosmopolitan surveyed 1,000 unmarried women in 2013 on all things birth control. The results found 49 percent of women ages 18 to 29 did not consistently use contraception — yet each of the 1,000 unmarried women surveyed said they did not want to get pregnant at that time in their life. So why the disconnect? One in four women surveyed admitted they were scared by the medical warnings touted on TV commercials.
These warnings include vaginal bleeding, nausea, breast tenderness, headaches, weight gain, changes in mood, and libido. Two recent studies even suggest taking the pill for five years can increase risk for Crohn’s disease (in women with a genetic predisposition) and thin out two brain regions, the lateral orbitofrontal cortex and the posterior cingulate cortex.
Dr. Vanessa Cullins, vice president of external medical affairs at PPFA, told Medical Daily the pill is one of the most studied forms of medication available, with the general consensus being it’s very safe for women to take. At the same time, she added, all medications have some risks. This is why she recommends women talk with their health care provider about the risks and benefits attached to any method.
“Women should feel free to try different methods — birth control methods are not one-size-fits-all,” Cullins said. “A method that’s perfect for one woman may not be right for another, and for most women, you may need a different method at different points in your life.”
Intrauterine Devices (IUDs) Are Effective
A Centers for Disease Control and Prevention (CDC) report found IUDs and implants, which are both inserted by a doctor, are considered the most effective forms of birth control. However, the CDC added 43 percent of sexually active teens are still looking to birth control pills and condoms. Both these methods are proven to protect against pregnancy and STDs, but they’re also proven to be easily forgotten. Going back to the 2013 survey of unmarried women, one in four respondents said taking something every day “doesn’t work for me.”
IUDs didn’t always have a great reputation. Though they were invented in 1909, certain IUDs produced in the late 70s were found faulty, causing certain medical problems and pregnancies. Not only did this prompt women to return to their diaphragms, but it prompted official investigations into the device. Ultimately, in the 2000s, IUDs were redeemed and are now considered the fastest growing form of birth control, especially among younger women.
“I think the old myths and biases against IUDs are falling away, and women are becoming more aware of how safe and effective modern IUDs are,” Cullins said. “We’re also seeing more providers being educated on IUD safety and trained on how to properly insert and remove IUDs, as well as more marketing from IUD manufacturers.”
Cullins added PPFA has found the prevalence of IUD and implant contraception has grown 91 percent, with IUD use in particular increasing 57 percent.
Restricted Access Can Be Harmful
Hobby Lobby convinced the Supreme Court their company’s religious beliefs should exempt them from the Affordable Care Act’s contraceptive mandate, in which birth control is seen as basic and preventive health care. It seems now insurance companies are following suit and trying to limit the medical care provided under the ACA. A Kaiser Family Foundation report just found several insurance carriers "require cost sharing, decline coverage, or otherwise limit coverage of certain contraceptive methods," including but not limited to popular and effective IUDs.
“Some of the most effective methods of birth control are also the most cost prohibitive,” Cullins said. “IUDs are the most cost effective method of birth control since they can provide coverage for up to 12 years — but upfront cost can be a barrier for some women interested in using an IUD. That’s why the [ACA] is so important. An IUD typically costs between $500 and $1,000, which covers the exam, insertion, and a follow-up visit.”
To Cullins, the ACA is the single biggest advancement in women’s health in a generation. About 48.5 million women have benefitted from the ACA’s preventive services without any out-of-pocket costs — and in 2013 alone, Cullins cited birth control saved women and their families $483 million.
A study from the University of California, San Francisco found for teens, birth control sold over-the-counter significantly reduces unwanted pregnancies. Researchers estimated if women could buy, say, birth control pills at a pharmacy without a prescription, up to 12 percent more women would use the pill. This is partially why emergency contraception recently became available to every woman.
"When a woman fears she might become pregnant after her contraceptive has failed or she has had unprotected sex, she needs fast access to emergency contraception, not delays at the pharmacy counter," Cullins said. "The age restrictions on over-the-counter emergency contraception are simply not supported by science — having emergency contraception stocked on store shelves means more women than ever will be able to prevent unintended pregnancy."
Education Remains Key
Perhaps more important than accessible and affordable contraception is accessible and affordable education. Cullins referred to data from a 2012 Contraceptive CHOICE study showed birth control counseling lead to significantly lower rates of unintended pregnancies. Researchers followed more than 9,200 women and teens for four years and found when women have information about the full-range of birth control methods and full-coverage of the cost of the method they select, many will choose IUDs or implants.
"As the leading women’s health care provider and advocate, Planned Parenthood knows that women need access to the full range of contraceptive methods," Cullins said. "Access to birth control without a copay has clear health and economic benefits for women and their families; it’s simply unacceptable that women are still being denied insurance coverage for birth control as required by federal law."



























