Eye Infections Often Resistant To More Than One Drug, But Antibiotic Resistance Is Slowing Down Overall
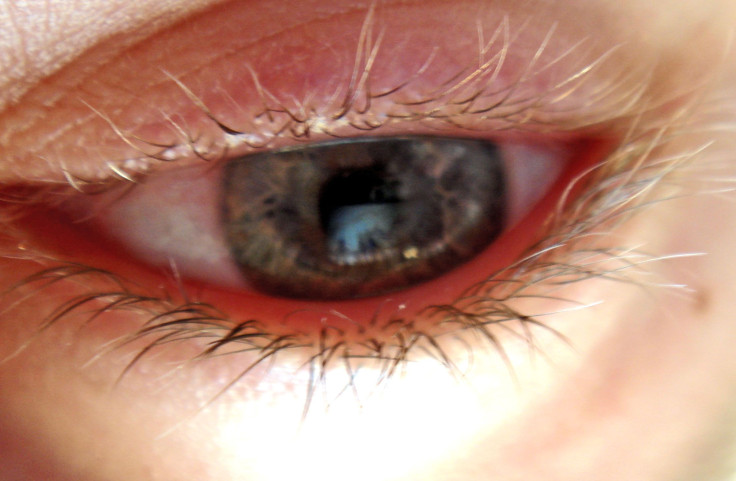
Antibiotic resistance is a problem that plagues even commonplace eye infections, according to a new comprehensive study published Thursday in JAMA Ophthalmology.
Analyzing more than 3,000 bacterial samples over a five-year-period — diligently swabbed from the infected eyes of actual patients — the study authors found that the resistance rates of certain germs has reached to nearly 50 percent of the population. Worse still, these superbugs often have resistance to at least 3 additional classes of antibiotics, making them multidrug resistant. Yet, not all the news is bad, since the researchers also found that resistance rates haven’t markedly increased from 2009 to 2013, the length of the study.
The Eyes Have It
Known formally as the Antibiotic Resistance Monitoring in Ocular Microorganisms (ARMOR) Surveillance Study, the program is the “only ongoing nationwide antibiotic resistance surveillance program specific to ocular pathogens,” according to the authors.
In its five years of existence, the ARMOR study has enlisted 72 clinics across 36 states to send in samples of the most common pathogens known to cause eye infections, including Staphylococcus aureus, a bacteria widely feared by doctors due to its rapid resistance in a relatively short period of time. The most common iteration of resistant S. aureus is called methicillin-resistant Staphylococcus aureus (MRSA), though that term actually describes staph bacteria that are resistant to any number of beta-lactam antibiotics (including penicillin), and not merely methicillin, which is no longer used.
Sure enough, the authors found that nearly half of the S. aureus samples were MRSA, as were the samples containing related bacteria known as coagulase-negative staphylococci (CoNS). Together, S.aureus and CoNS bacteria accounted for two-thirds of the total samples collected (3,237). The methicillin-resistant strains were similarly likely to harbor resistance to three other classes of antibiotics tested against them, which included fluoroquinolones, aminoglycosides, and macrolides.
All told, a third of S. aureus and CoNS samples were multidrug resistant, and resistant strains were most likely to appear in the eyes of the elderly, an expected finding, according to the researchers, given that they often spend time in nursing homes and hospitals, which are known to be laden with antibiotic-resistant bacteria. These rates are similar to those found among bacteria that infect the body elsewhere, as well as earlier research looking at eye infections.
On the bright side, the authors found that there were mostly low levels of antibiotic resistance seen among the other pathogens they tested, a hard-to-pronounce group which includes Haemophilus influenzae, Pseudomonas aeruginosa, and Streptococcus pneumoniae. Additionally, none of the samples were resistant to vancomycin, a drug often considered a last resort medication for resistant bugs, albeit one that comes with severe side effects.
Most importantly, and in line with other recent research, the authors found no increase in the resistance rate of any one germ over the past five years, and even a slight reduction of resistance to the drug ciprofloxacin among CoNS bacteria. “These findings are promising and may reflect improved antibiotic stewardship,” the authors wrote. “Indeed, programs advocating judicious antibiotic use by limiting overprescription of antibiotics, cycling between antibiotic classes, and using combination therapies have led to a decrease in resistance among bacteria involved in systemic infections and are likely having a similar impact among bacteria causing ocular infections.”
While their findings are overall promising, the authors explained that currently, it can take doctors several days to determine whether any bacterial infection is resistant to antibiotics, including those involving the eye. Until more rapid diagnostic methods are available, they hope their research can serve as a roadmap to better “guide the empirical treatment of ocular infections.”
Source: Asbell P, Sanfilippo C, Pillar C, et al. Antibiotic Resistance Among Ocular Pathogens in the United States. JAMA Ophthalmology. 2015.
Published by Medicaldaily.com



























