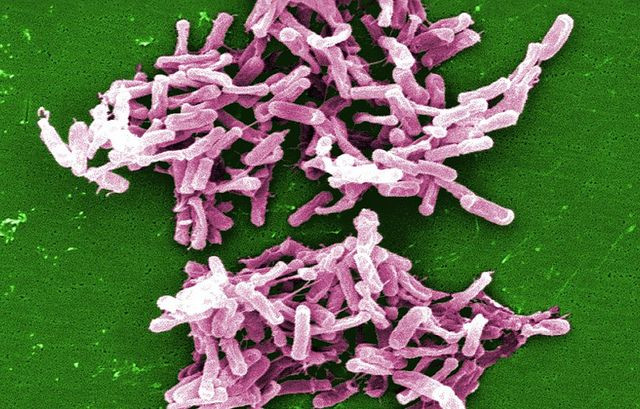
Fecal Transplant For C. Difficile Infection Works Equally Well If Fecal Matter Is Frozen Or Fresh
Patients requiring fecal microbiota transplantation (FMT), otherwise known as fecal transplant, as a result of Clostridium difficile infection may be heartened to learn that the fecal matter they receive can either be frozen or fresh, a new pilot study finds.
Ever since antibiotics gained widespread use in physicians’ treatment regimens, somewhere around the year 2000, hypervirulent strains of C. difficile have emerged. The overuse of these antibiotics deadens their effect, giving bacteria time to adapt and become resistant. Patients who suffer from C. difficile infection must undergo FMT in order to restore an ecosystem of healthy gut bacteria that may have been flushed away in treatment.
Each year, C. difficile infection results in nearly 250,000 people needing hospital care, with at least 14,000 deaths occurring. To combat the infection’s chronic diarrhea, which results from the imbalance of bacteria in the host’s digestive system, doctors typically need to replace the fecal matter that resides within the person with donor materials that have healthier concentrations of bacteria. Traditionally, these transplants were achieved through colonoscopy. However, the invasiveness of the procedure, mixed with the uncomfortable preparatory flushing the day before, makes it unattractive to both doctors and patients.
The new study offers a solution. "We found that delivery of a frozen, stored inoculum through a nasogastric tube is safe, acceptable to patients, and as successful as delivery by colonoscopy,” said Dr. Elizabeth Hohmann, senior author of the Mass General Hospital Infectious Diseases Division, in a statement. In other words, patients had a tube stuck down their nose that delivered frozen poop into their stomachs. And surprisingly, they had no problems with it.
In fact, out of the 20 people enrolled in the study, a success rate was achieved in 90 percent of cases, with an insignificant difference between the colonoscopy group and the group given a nasogastric tube (NGT). If the first infusion did not resolve the infection, patients were given the option of receiving a second infusion. Of the six people whose infections persisted, one person rejected the option and the five remaining all chose NGT. One subject, however, took matters into his own hands and was found to be self-delivering fecal enemas courtesy of his roommate.
"We certainly don't recommend 'home brew' FMT, since it's very important to screen donors properly,” Hohmann warned. “In addition, while some people may be comfortable using stool from a spouse or other intimate partner, many older patients might not have such a donor who is healthy enough to donate safely."
Frozen fecal matter has another upside, the researchers point out. Whereas readily available materials for colonoscopies can be expensive to acquire, given the time and money used to recruit and screen potential donors, frozen matter can be stored in bulk for later use. The team’s current study, which produced a follow-up trial on 11 patients that had a comparable success rate, may lead to future research that eliminates the need for FMT altogether. If the technology allows it, the team hopes to develop an easily digested capsule that produces the same bacteria-balancing effect.
"It's been very gratifying to be able to help these patients, some of whom have been sick for a year or two," Hohmann explained, adding that it’s rare to see any procedure, however small, achieve a 90 percent success rate for patients. "They have told us this has been life changing for them and that they have gotten themselves back to normal.”
Source: Youngster I, Sauk J, Pindar C, et al. Fecal Microbiota Transplant for Relapsing Clostridium difficile Infection Using a Frozen Inoculum From Unrelated Donors: A Randomized, Open-Label, Controlled Pilot Study. Clinical Infectious Diseases. 2014.
Published by Medicaldaily.com



























