First Hepatitis C Genotyping Test Approved By FDA, Heralding Personalized Treatment Before Curing Drug Introductions
Hepatitis C has been called a silent killer because it can lay and wait in dormancy, for years. With 3.2 million people in the U.S. infected, 75 percent of which are baby boomers, and the vast number unaware they are ill, treatments needs to be implemented quickly. Because the disease has been so difficult to treat and with potential drugs months away from hitting the market, a new hepatitis C genotyping test test to determine which subtype of the virus a patient has is a vital piece to the puzzle.
Today the U.S. Food and Drug Administration (FDA) approved one test called Genotype II, made by Abbott Laboratories, that can distinguish between different genotypes, or strains, of the hepatitis C virus using a sample from a patient's blood. The genotypes that will be able to be identified are 1, 1a, 1b, 2, 3, 4, and 5, with genotype 1 being the most prevalent in the U.S. and the most difficult to treat. The importance in knowing which genotype of the virus a patient has rests in the treatment. Different genotypes of the virus respond to drug treatments differently. Additionally, with drugs that can cure the disease in as little as six weeks, such as the Direct Acting Antivirals (DAA's) sofosbuvir and simeprevir currently under review by the FDA, and approval set for later this year, knowing which genotype will be key to ending this silent epidemic.
"Tests such as this one can help physicians gain an understanding of a patient's HCV status," said Alberto Gutierrez, Ph.D., director of the Office of In Vitro Diagnostics and Radiological Health in FDA's Center for Devices and Radiological Health. "Along with other clinical factors, the particular type of HCV is an important consideration in aiding health care professionals in determining if and when to initiate treatment and the appropriate type of treatment."
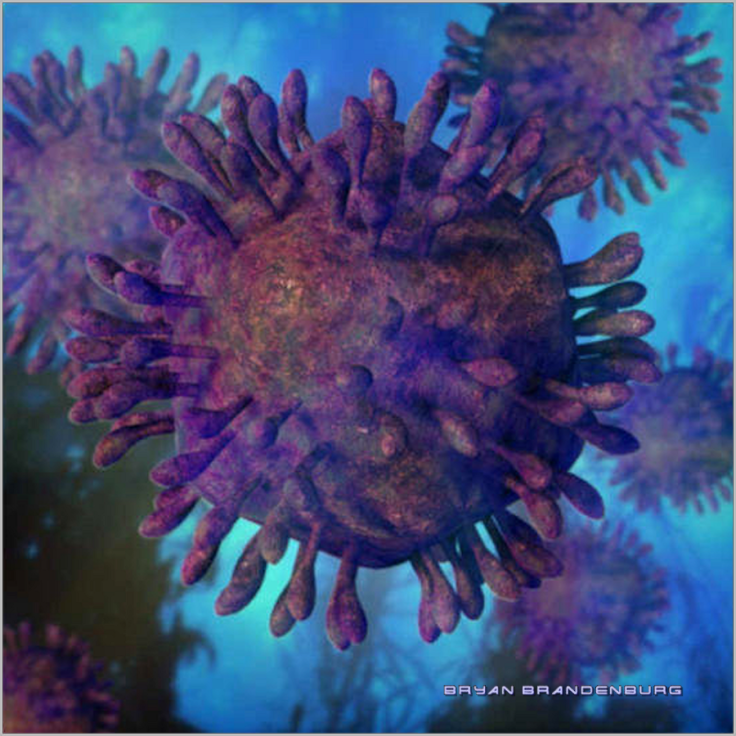
Hepatitis C is a virus that infects cells of the liver, and long-term infection can lead to scarring of the liver as well as liver cancer and failure. Accordign to the Centers for Disease Control and Prevention (CDC), 15,000 Americans die as a result of the infection yearly in the U.S. Hepatitis C is spread through blood and body fluid contact, with intravenous drug users at the highest risk because of needle sharing. The new test is approved only to determine which genotype an infected patient has, not to diagnose the presence of the virus.
"Hepatitis C is known as the silent killer as many of the symptoms go unnoticed. When patients are identified, determining their specific genotype is important to ensuring they receive the treatment that will prove to be most effective. The introduction of this test for broad use in the U.S. is a significant advancement in helping to address an important public health issue," said HIV and viral hepatitis expert, Carol Brosgart, M.D., Clinical Professor of Medicine, Division of Global Health, University of California San Francisco in a press statement.



























