Gender Income Gap Among Doctors At $56,000: Unequal Opportunity Or Personal Preference?
As a beacon for gender equality, the wage gap between men and women has seen considerable leaps forward in the last few decades. Still, despite legal measures, such as the Lilly Ledbetter Fair Pay Act, and pockets of social activism, many argue the fight for equal pay is still a worthy pursuit. A recent study reveals the fight may be further uphill than once thought, as the gender income gap hasn’t budged among doctors since 1987.
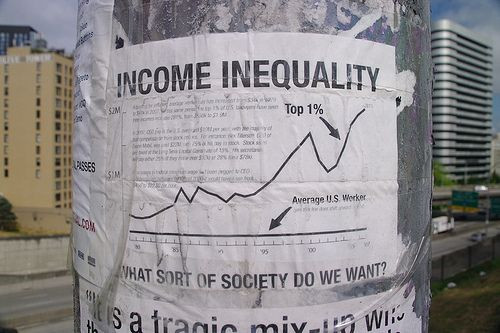
Income Inequality In The Hospital
Income inequality has as many moving parts as it does people fighting for either side of the argument: activists fighting for greater equality point toward inaccessible opportunities for women, which cause implicit forms of bias in the system. Less concerned people argue that activists discount the role of occupation in the gap, that women take up different, lower paying roles, which create a natural and fair wage gap. Among doctors, the issue is no less controversial, as a recent study from Harvard Medical School's Department of Health Care Policy found that the average male doctor earned about $221,000 from 2006 to 2010, while the average female doctor earned $165,000.
Researchers looked at nationally representative survey data from 1987 to 2010. Despite finding a shrinkage in inequality among non-healthcare workers, income among doctors and nurses retained its differences.
"There is something that's intrinsically going on within the physician workforce," said Dr. Anupam B. Jena, the study's senior author. “We would have suspected that the gender gap between males and females would have converged somewhat over the years, and what we found was that it was relatively constant."
Nearly 6,300 doctors and 32,000 other healthcare workers comprised the study, which analyzed account hours worked and years of experience. The researchers did not take physician specialty into account, something that many critics argue is vital to understanding the root of income inequality.
"I view that as the big question that remains unanswered: what can we really say about how much of this is a choice that physicians are making, a willing trade-off between making more money and having a more reasonable balance of work and life?" Anthony Lo Sasso, a health policy and economics researcher from the University of Illinois at Chicago, told Reuters Health.
"I think it really gets at whether we want to label this difference as a problem or not,” he added.
The researchers’ study cross-referenced data between 2006-2010 with 1987-1990 data. They found a 25 percent difference among male and female doctors and healthcare workers in the more recent data set — five percentage points greater than the earlier data. Dentists maintained roughly a 40 percent difference, pharmacists an 11 percent difference, and nurses a six percent difference, the team reported in JAMA Internal Medicine.
Meanwhile, salaries in outside professions saw the gap narrow to 15 percent between 2006 and 2010, compared to a 28 percent gap in years prior.
Public Problem Or Personal Choice?
These differences specific to the healthcare industry could have their roots in both specialty and levels of access, as some argue the two cannot help but be related. When certain biases and discrimination push male doctors toward one profession and women doctors toward another, certain patterns become normalized. Throw child care into the mix and female doctors begin to take considerable chunks of time off compared to their male counterparts. They may hold the same job, but due to lifestyle choices — or obligations, in some cases — the income gap continues to widen.
"It could very well be the case that male and female pediatricians and male and female surgeons earn the same amount of money. But if it's more difficult for females to enter surgery, then their access to higher-paying fields would be lower," Jena, also from Massachusetts General Hospital in Boston, told Reuters Health. “Whether we call this discrimination or bias…I think that's probably some component of it.”
Both Jena and Sasso agreed that the differences in income need more attention to know whether female doctors are hitting a glass ceiling or making personal choices to enter certain professions, which happen to pay less, and work fewer hours. The best course of action, Jena argued, is removing any possibility that access is the cause.
"If opportunities are equally accessible, and women continue to choose certain specialties because of lifestyle reasons, that's totally fine," he said. "But we have to make sure those opportunities exist."



























