Genetic Parkinson's Mutated Brain Cells Made in Lab, A Step Closer to Cure
Scientists have successfully replicated the genetically caused Parkinson’s disease brain nerve cell in the laboratory formed from skin cells, a breakthrough researchers believe will give them the ability to precisely examine how mutations in the parkin gene affects 10 percent of patients with Parkinson’s.
Researchers from the University of Buffalo said that their findings may reveal potential new drug targets for the disease as well as a screening platform for discovering new treatments that imitates the protective functions of parkin.
Human brain nerve cells have generally been inaccessible or off-limits because they are located deep in the brain and live in a complex web of networks and animal models generally lack the parkin gene, but recent stem cell breakthrough overcomes the formidable hurdle in research on Parkinson’s and other neurological disorders.
“Before this, we didn’t even think about being able to study Parkinson’s disease in human neurons,” said the study’s lead author, Jian Feng, PhD, professor of physiology and biophysics in a statement released by the University on Tuesday.
Feng and his research group used a technique that had already been successfully tested by other scientists called induced pluripotent stem cells (iPSCs).
In 2007, Japanese researchers announced that they were able to convert human cells to iPSCs, which like embryonic stem cells, could be made into nearly any cell in the body.
“This new technology was a game-changer for Parkinson’s disease and for other neurological diseases,” Feng said. “It finally allowed us to obtain the material we needed to study this disease.”
Feng and his team were the first researchers to use human neurons to investigate parkin’s role in Parkinson’s, and they found that the parkin mutations interrupts precise dopamine functionality and produced more free radicals that destroy dopamine neurons which leads to the brain disease.
Feng and his team believe that human neurons have unique vulnerabilities because the large size of the brain uses more dopamine to support neural computation needed for bipedal movement, compared to quadrupedal movement of almost all other animals.
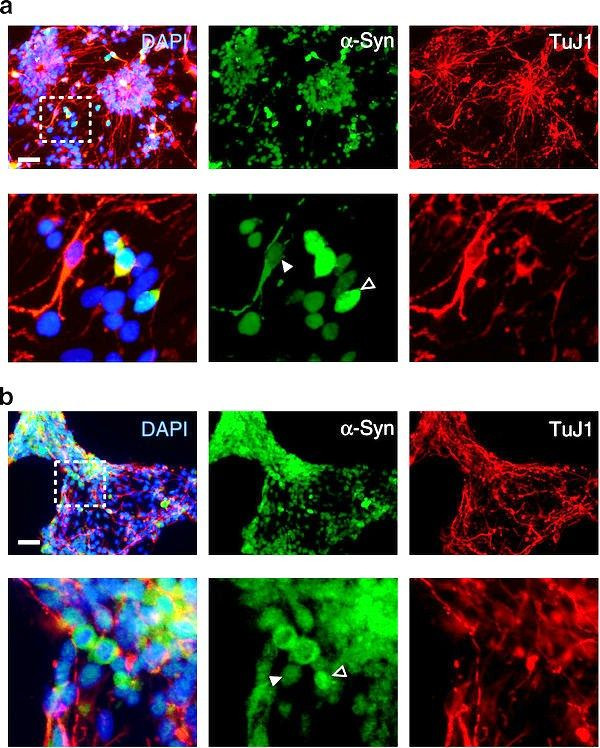
Researchers reverse-engineered human neurons from skin cells taken from four subjects: two with a rare type of Parkinson’s disease caused by the parkin mutation and two healthy control subjects, and found that once parkin mutates, it can no longer control the action of dopamine that supports the neural computation required for movement.
Specifically, parkin mutations prevent it from its normal function of securely controlling the production of monoamine oxidase (MAO), which catalyzes dopamine oxidation.
“Normally, parkin makes sure that MAO, which can be toxic, is expressed at a very low level so that dopamine oxidation is under control,” Feng explained. “But we found that when parkin is mutated, that regulation is gone, so MAO is expressed at a much higher level.
“The nerve cells from our Parkinson’s patients had much higher levels of MAO expression than those from our controls. We suggest in our study that it might be possible to design a new class of drugs that would dial down the expression level of MAO,” Feng added.
Feng noted that one of the drugs currently used for Parkinsons inhibits the enzymatic activity of MAO and has been demonstrated in clinical trials to slow the progress of the disease.
Researchers have already shown that they can reverse the defect of the mutated parkin by inserting a normal parkin gene into diseased neurons.
Dr Michelle Gardner, research development manager at Parkinson's UK, told BBC that the new study was exciting because it offered a new way to explore this genetic form of Parkinson's.
The findings were published in the Feb. 7 issue of Nature Communications.
Published by Medicaldaily.com



























