Gonorrhea Becomes More Resistant To Last-Line Antibiotics, But New Guidelines May Stop Its Spread
Although surveillance data from the UK indicates that drug-resistant gonorrhea has been on the rise, recent changes to prescription guidelines appear to be effective in halting its spread. Published in The Lancet Infectious Diseases, the study aimed to evaluate the effectiveness of cephalosporins, the remaining class of antibiotics used to treat gonorrhea.
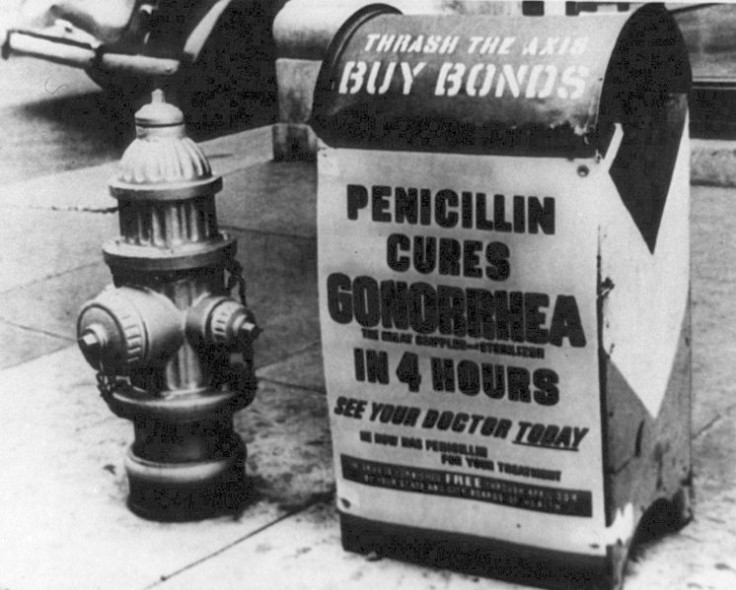
Gonorrhea has been acquiring resistance to antibiotics for as long as they have been in use, rendering classes of drugs completely ineffective in treatment. In the 1940s, gonorrhea developed resistance to sulfonamides, then to penicillins and tetracyclines in the 1970s and 1980s. Most recently in 2007, gonorrhea became less susceptible to fluoroquinolones, leaving cephalosporins the sole class of antibiotics for treatment.
Researchers analyzed Neisseria gonorrhea bacteria collected from patients through Public Health England's Gonococcal Resistance t Antimicrobials Surveillance Programme (GRASP) from 2007 to 2011. Samples were tested for resistance to cefixime, a type of cephalosporin, by determining the cefixime minimum inhibitory concentrations. Basically, researchers wanted to measure how high a concentration of the drug cefixime is required to inhibit the growth of the bacteria.
They found that a greater percentage of gonorrhea samples required high concentrations of the drug to fight it, indicating that the bacteria have become more resistant to cefixime. In 2007, 1.5 percent of samples had become more resistant, rising to 17.1 percent in 2010, then falling to 10.8 percent in 2011. A closer look at each of the bacterial isolate's isolates indicate that they were closely related genetically.
Further analysis showed that the resistant bacteria were more prominent in patients who were homosexual men, older than 19 years of age, HIV-positive, and had higher rates of partner change. This means gonorrhea that is less susceptible to cefixime treatment is circulating around a "largely distinct and highly active sexual network," the authors hypothesize. Forms of gonorrhea more susceptible to cefixime treatment were found in heterosexual populations.
Although the overall rise across the five years of surveillance is alarming in itself, the drop in cefixime-resistant samples from 2010 to 2011 indicates that the national treatment guidelines adopted during that time may be effective in stopping the spread of the disease. Currently, UK guidelines state that gonorrhea should be treated with high-dose ceftriaxone (a broad-spectrum cephalosporin) and azithromycin, another type of antibiotic, before the bacterial resistance reaches a certain threshold.
"Although we cannot attribute causality to this observation, the progressive accumulation of isolates with decreased cephalosporin susceptibility from 2007 to 2010 seems to have been delayed or reversed", the authors write.
While data was only collected in the UK, these findings present a glimmer of hope in stemming the rise of drug-resistant gonorrhea in the U.S., as similar prescription guidelines of using ceftriaxone combined with azithromycin against gonorrhea were implemented around the same time.
Among notifiable infections reported to public health authorities, gonorrhea is the second most common infection, with 321,849 cases documented in 2011. An estimated 700,000 additional cases are suspected, as gonorrhea may be asymptomatic. Around the world, the World Health Organization estimates 106 million new cases of gonorrhea each year.
Gonorrhea is usually transmitted through vaginal, anal, or oral sex with an infected person. Symptoms include pain and burning upon urination, or unusual discharge from the genitalia. If left untreated, gonorrhea infection can lead to infertility problems in women and pelvic inflammatory disease. Infants born to mothers with gonorrhea could acquire blindness from exposure.
Public health authorities in the U.S. and elsewhere worry about the possibility of gonorrhea becoming resistant against cephalosporins, as few other antibiotics remain in the pipeline. Gonorrhea resistant to all treatments would be devastating for society, hurling modern science back to the dark ages before the widespread use of antibiotics.
Luckily, one last defense against gonorrhea infection will remain: the condom. As with many sexually transmitted diseases, using condoms during sexual intercourse greatly reduces the risk of infection.
For more information on how to protect against gonorrhea and other sexually transmitted infections, consult the Centers for Disease Control website.
Sources: Kirkcaldy RD, Bolan GA, Wasserheit JN. Cephalosporin-resistant gonorrhea in North America. JAMA. 2013.
Ison CA, Town K, Obi C, Chisholm S, Hughes G, Livermore DM, Lowndes CM, on behalf of the GRASP collaborative group. Decreased susceptibility to cephalosporins among gonococci: data from the Gonococcal Resistance to Antimicrobials Surveillance Programme (GRASP) in England and Wales, 2007-2011. The Lancet Infectious Diseases. June 2013.



























