Laser Monitoring For Diabetes Could Replace Traditional Blood Glucose Tests

Pesky pinpricks may soon be a thing of the past for diabetes patients, if new research from Princeton University keeps on its current trajectory. Engineers have developed a laser capable of checking sugar levels under the skin without having to pierce it first.
Medical science has made enormous leaps in recent decades, but some procedures have yet to fully catch up. Prostate exams, with their primitive gloved fingers, are a good example. For diabetics, the daily task of drawing blood just to get one reading can be a nagging chore, a routine reminder that something’s amiss. The latest project at Princeton is still the size of a desktop, but researchers believe the laser’s size may be as great as its potential.
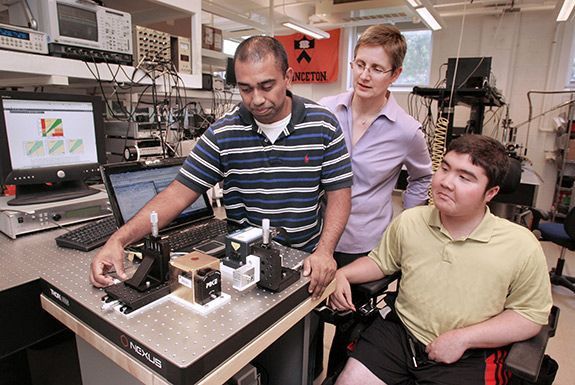
“We are working hard to turn engineering solutions into useful tools for people to use in their daily lives," said Claire Gmachl, a professor of electrical engineering at Princeton and the project’s senior researcher, in a statement.
The researchers describe their findings in a report published in the journal Biomedical Optics Express. The team fires the mid-infrared laser at a person’s palm without causing damage to the skin. The laser then passes through the skin cells and gets absorbed by the sugar molecules floating inside. How well the laser is absorbed gives the researchers a proxy for judging blood sugar levels.
The method is imperfect, but so are blood glucose monitors. Federal regulation requires traditional reading methods to produce a blood-sugar reading within 20 percent of the actual level. In their lab tests, the highest accuracy the Princeton engineers achieved was within 16 percent of the actual levels.
The trick to the laser’s success comes in its frequency. Most devices rely on “near-infrared,” which refers to the rays’ proximity to the band of visible light on the spectrum. While able to penetrate more deeply and accomplish the same water-piercing task of mid-infrared rays, for simple blood glucose monitoring they’re often too strong, interacting with acids and chemicals in the skin and potentially causing damage.
Mid-infrared rays offer the benefit of absorption but without the collateral damage; however, their drawback is in the power they require to operate stably. So the team had a challenge: How do they harness the power of mid-infrared lasers in a concentrated, practical way?
They arrived at what is known as a quantum cascade laser. As opposed to many other lasers, for which the material making up the stuff of the laser determines the frequency, quantum cascade lasers use electrons passing through a “cascade” of semiconductor layers to generate their beam. The net effect is a greater ability to manipulate the laser’s frequency, thus, achieving a mid-infrared range.
"Because the quantum cascade laser can be designed to emit light across a very wide wavelength range, its usability is not just for glucose detection,” Gmachl said, “but could conceivably be used for other medical sensing and monitoring applications.”
After giving their subjects 20 jelly beans to boost their glucose levels, the team fired their lasers at each participant’s palm. The results showed the laser made more errors than traditional testing methods, but still fell within the range for clinical acceptance — a result the team considered a victory. "It works now but we are still trying to improve it," said Sabbir Liakat, a graduate student in electrical engineering.
With more tinkering, the team hopes to reduce the laser in size to the point where it can be brought to doctors’ offices for clinical use. Further down the line, they envision a portable consumer model that, to the delight of diabetics everywhere, can finally stop the bleeding.
Source: Liakat S, Bors K, Xiu L, Woods C, Doyle J, Gmachl C. Noninvasive in vivo glucose sensing on human subjects using mid-infrared light. Biomedical Optics Express. 2014.



























