Mad Scientist: 6 Scientists Who Were Dismissed As Crazy, Only To Be Proven Right Years Later
All truth passes through three stages. First, it is ridiculed. Second, it is violently opposed. Third, it is accepted as being self-evident. – Arthur Schopenhauer
As a scientist, it’s important to be skeptical, lest quackery and “crackpottery” freely seep into scientific acceptance. But sometimes the scientists who are dismissed as quacks and crazies turn out to be right in the end, often vindicated by posthumous awards and even Nobel prizes. Here are some famous doctors and medical researchers who were considered nuts when they first introduced their findings to the scientific world, but were later found to be right — they changed the world for the better.
William Harvey

William Harvey was a 17th century English physician who was the first to describe blood circulation to the heart, brain, and body in complete detail — though it took years for the mainstream scientific community to accept it. In 1628, he published De Motu Cordis, or “On the Motion of the Heart and Blood,” at a Frankfurt book fair. The book describes the structure of the heart and arteries, and posited for the first time that blood passed through the heart, not the liver as previously believed.
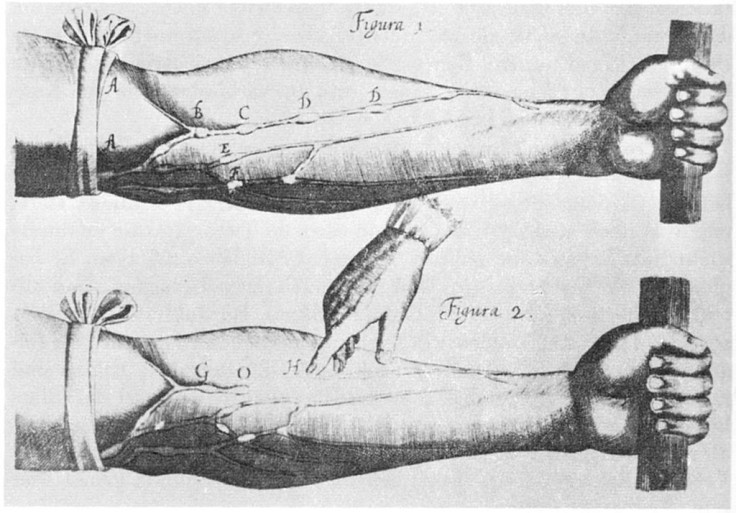
However, it was Galen, a 2nd century philosopher and physician who still held the authority on most matters of physiology, including circulation. He believed that the liver creates blood from food, then sends it through the left side of the heart and lungs. Though most of his writings were incorrect, people still held strong to his beliefs, even 1,500 years later. As a result, Harvey’s findings were ridiculed, and many doctors in the 17th century noted that they would “rather err with Galen than proclaim the truth with Harvey.”
In his later years, ostracized by the scientific world, Harvey became a recluse, living life in private and peace rather than launching again on what he called “the faithless sea.”
“Much better is it oftentimes to grow wise at home and in private,” Harvey reportedly said, “than by publishing what you have amassed with infinite labor, to stir up tempests that may rob you of peace and quiet for the rest of your days.”
Gregor Mendel

You probably remember Gregor Mendel from your elementary school science class. Known as the father of modern genetics, Mendel was a Moravian Augustinian friar who dabbled in crossbreeding of pea plants during his spare time. Though he may not necessarily have been considered a complete lunatic during his time, he wasn’t exactly well-known or respected for his experiments, either.
Mendel’s garden pea plants, which helped him come up with the words “recessive” and “dominant” in reference to genes, were largely kept to himself and not fully accepted until after his death. In the past, scientists had believed that traits were passed down to next generations through blending inheritance, in which they’re averaged and mixed together. Mendel died in 1884, but it wasn’t until several decades later — at the beginning of the 20th century — that his ideas came to be known as modern genetics.
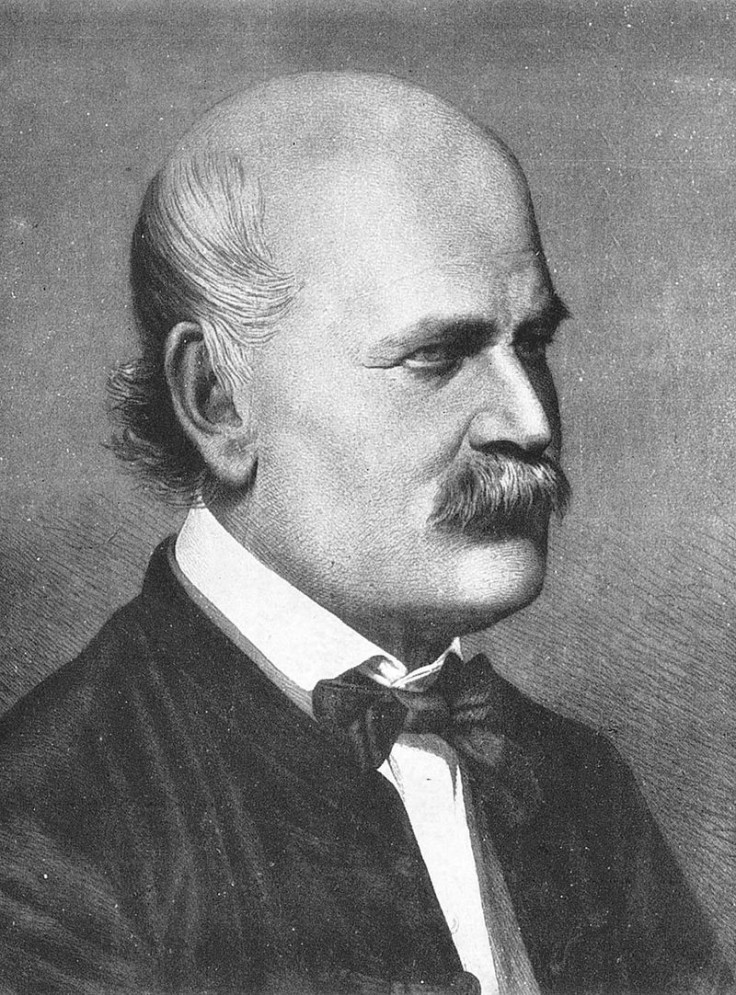
Ignaz Semmelweis
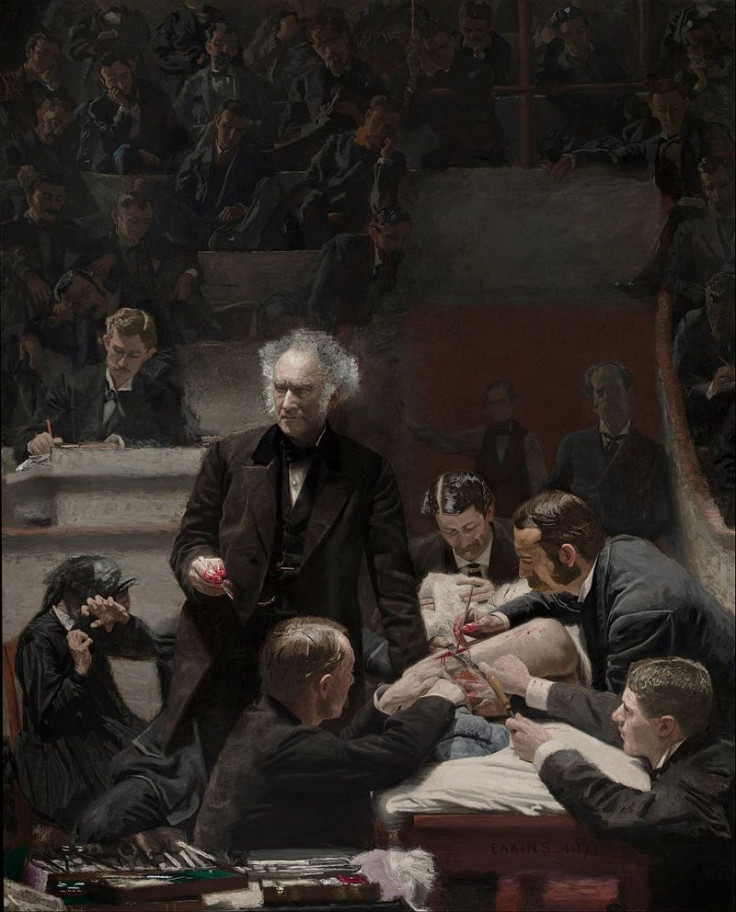
Basic hygiene — like washing your hands or using antibacterial sanitizer — is now commonplace, and considered protocol in hospitals. But before the 19th century, doctors weren’t aware that bacteria spread through lack of sanitation. Infectious diseases were typically treated by bloodletting (the explanation being that the four humors needed to be balanced), and illness was believed to be caused by bad air. Medical students often went straight to birthing babies after handling contaminated cadavers without washing their hands.
Ignaz Semmelweis was a Hungarian physician working at the Vienna General Hospital in the 1840s. His tasks included inspections, teaching, and record-keeping. At the time, the hospital had a particularly bad reputation for maternal mortality due to puerperal fever, with a 10 percent death rate among new mothers. Another nearby hospital only had a 4 percent death rate, so Semmelweis set out to pinpoint what was causing the spread of the fever.
He noticed that the Vienna General Hospital’s medical students went from autopsying cadavers straight to birthing babies. Though he didn’t know anything about germs, he assumed it was a lack of cleanliness causing unnecessary deaths. When he had doctors and midwives wash their hands in chlorine lime solutions, the mortality rates went down to 1 to 2 percent.
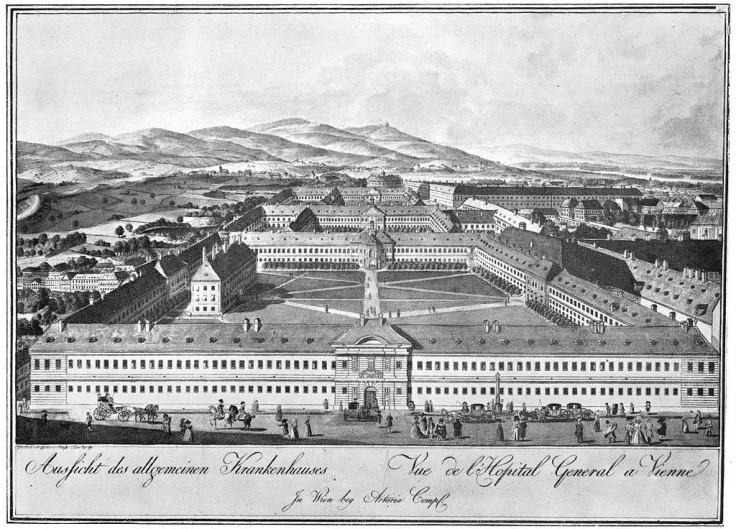
It seems straightforward enough, but news of washing hands didn’t go over well in the rest of Europe. Many doctors were offended that Semmelweis saw them as dirty, their egos leading them to believe that it couldn’t be their uncleanliness that caused disease. And because Semmelweis never published an official report on why sanitation was life-saving, the medical world completely rejected him, viewing him as an embarrassment.
The rejection drove him to alcoholism, depression, and isolation. He even penned several letters lashing out at his critics, noting that the doctors who rejected his work were “irresponsible murderers” and “ignoramuses.” Toward the end of his life, he was sent to a mental asylum, where he died forgotten by his peers. Decades later, germ theory immerged with the likes of Louis Pasteur and Joseph Lister practicing medicine with hygienic procedures, proving that Semmelweis’ idea indeed saved lives.
William B. Coley
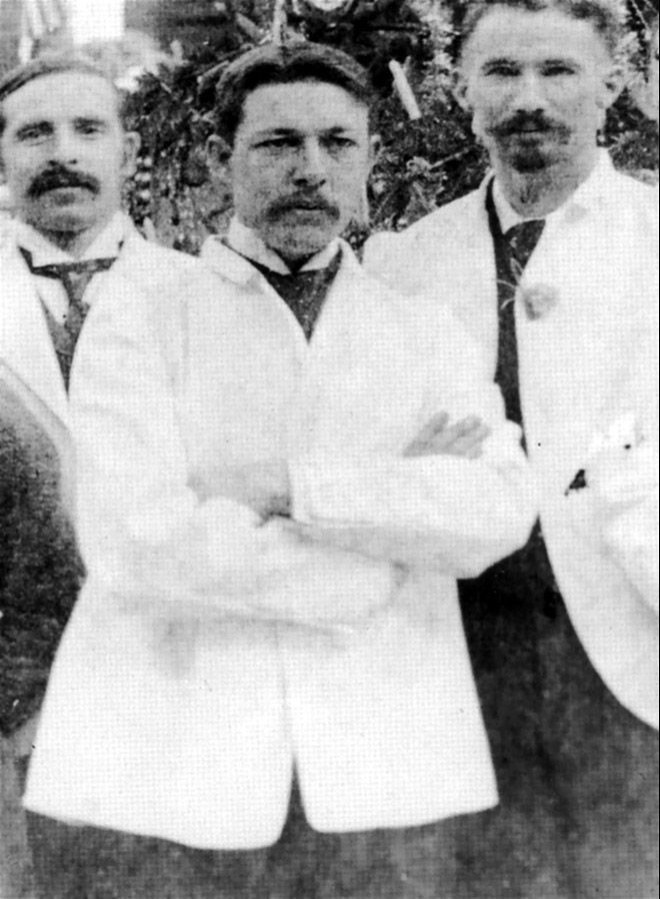
In the late 1800s, standard cancer treatment involved surgically removing tumors or cancerous tissues; there was no chemotherapy, radiation, or cancer drugs. But one man, William Coley — a cancer researcher and bone surgeon who worked at New York Cancer Hospital — stumbled upon a strange discovery that would pave the way for modern immunotherapy, various trajectories of cancer treatment that involve triggering the immune system to attack cancer cells.
One of Coley’s patients began recovering from cancer after he was infected with Streptococcus pyogenes bacteria, the microbe that causes strep throat. It was this event that led Coley to theorize that post-surgical infections actually helped defeat cancer by mobilizing the immune system against it. In the 1890s he experimented with what became known as Coley’s toxins — mixtures of dead bacteria, particularly streptococcus, injected into cancer patients to trigger their immune systems. He kept a series of case reports on it, but most of his scientific peers rejected the idea, writing it off as crazy and dangerous. He died in 1936, his work surpassed by chemotherapy and radiation, without ever knowing that Coley’s toxins would someday lead to the birth of modern immunotherapy.
Francis Peyton Rous

Francis Peyton Rous was a pathologist who discovered that certain viruses may play a role in the development of particular kinds of cancer. In 1911, while he was working at Rockefeller University in New York City, Rous noted that a sarcoma growing on a chicken could be transmitted to healthy chickens through a cell-free extract injection of chicken tumor. His findings were largely discredited, however, and he didn’t get rewarded for his work until over 50 years later, when he was given the Nobel Prize in Physiology or Medicine in 1966.
Rous’ early research on transmissible sarcomas “set in motion an entirely new way to study cancer; that is, through viruses,” a PLOS Blog states. “Although about 20 percent of human cancers are now thought to be transmissible through viruses, for the most part virus-caused cancers are confined to other animals. … However, the understanding that viruses can somehow carry cancer from one animal to another provided science a model with which to unravel how the transformation from normal to cancerous happens again.”
Barry Marshall

Barry Marshall may not have been a mad scientist, but he certainly submitted to crazy measures to prove his ideas. Starting out as an obscure Australian doctor, Marshall worked primarily on how Helicobacter pylori bacteria invaded the gut, and found that the bacteria caused both ulcers and stomach cancer.
Today, standard care for ulcers involves antibiotics to kill off the bacterial infection. But back in the 1980s, doctors believed ulcers were caused by stress. When Marshall argued antibiotics should be used to treat ulcers, his fellow physicians dismissed him, leaving him in a tight spot — he was unable to further his research as H. pylori only affects primates, and barred from experimenting on people.
That’s when Marshall did something crazy: He took H. pylori from a patient’s infected stomach, mixed it into a broth, and drank it. After falling ill, he biopsied his own gut, cultured the bacteria, and ultimately proved that H. pylori was indeed responsible for ulcers. Perhaps this is what earned him the nickname “the guinea-pig doctor.”
In an interview with Discover Magazine, Marshall noted that “[b]efore the 20th century, the ulcer was not a respectable disease. Doctors would say, ‘You’re under a lot of stress.’ Nineteenth-century Europe and America had all these crazy health spas and quack treatments.” Indeed, Marshall’s story is a reminder that not all symptoms or illnesses can be dismissed as stress or anxiety — and a determined scientist must often go to extremes to prove it in the midst of widespread resistance.



























