Men’s Health Week: Prostate Cancer Demystified, From Trouble Urinating To Biopsies

Each year, in the week leading up to Father’s Day, the Men’s Health Network celebrates Men’s Health Week. This year is the 20th anniversary, and what better way to spend it than by engaging in a frank discussion of the walnut-shaped gland surrounding a man’s urethra?
Prostate cancer is tricky. The prostate gland is nestled deep in the body, and few biomarkers are easy to attain without a doctor getting invasive. Even to this day, despite great leaps in artificial organ development, 3D printing, and stem cell cloning, a doctor’s best tool for assessing a man’s cancer risk is a well-greased index finger. Of course, this turns a lot of men off to getting their prostates checked, despite the fact that prostate cancer is the most common cancer among men.
The Low-Down
In 2010, according to the Centers for Disease Control and Prevention, just shy of 200,000 men in the U.S. were diagnosed with prostate cancer, and nearly 30,000 men died from the disease. What make prostate cancer so deadly are the hurdles prior to diagnosis. The initial symptoms will be a difficulty or hesitancy when urinating and possibly even a burning pain. This isn’t the most compelling evidence to have your prostate checked, of course, so the hurdle is a personal one.
But even if you get to a doctor, fearing that your persistent difficulty deserves more than a shrug, your doctor won’t necessarily have an easier time finding any possible cancer. The routine check experts typically recommend comes at age 50, when a man’s risk makes its first real jump. During the procedure, the doctor will perform a manual rectal exam in which he gauges the size, shape, and firmness of the gland — a process formally known as “palpating.” If the doctor feels any abnormality, such as possible tumors or enlargement, he or she will typically perform what’s known as a PSA (prostate-specific antigen) test.
Every man’s prostate produces PSA. It’s an enzyme that serves the main purpose of liquefying semen and allowing sperm to swim freely, and it just so happens to be a doctor’s first line of defense when it comes to diagnosing prostate cancer. But PSA tests aren’t perfect. They have a high sensitivity, but low specificity, which basically means they’re really good at detecting cancer, but good at discovering a bunch of useless information, too. So until a specialist takes numerous samples, cancer can’t necessarily be ruled out.
If the PSA test shows your levels are indeed too high, you’ll most likely be referred to a urologist, who will use a small needle to draw samples of the prostate’s actual tissue for direct examination under a microscope. This process, unfortunately, is invasive and can be painful. Keep in mind, however, that these tests aren’t arbitrary. They only exist to keep a deadly cancer at bay. Depending on the outcome of the biopsies, the specialist may order another round of biopsies or PSA tests, or take more advanced measures such as surgery to remove part or all of the prostate, or begin radiation or hormone therapy.
Research, Ahead
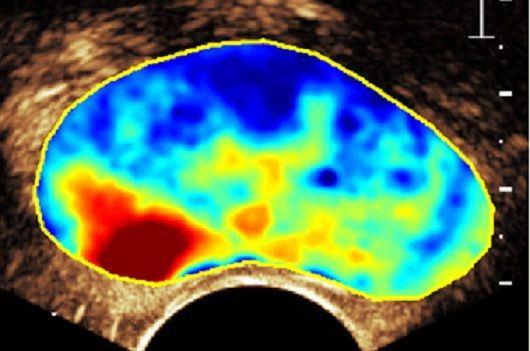
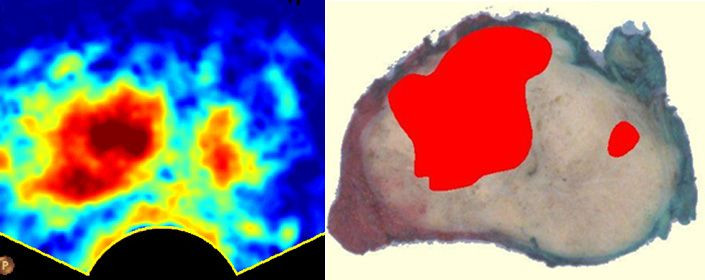
Because prostate cancer complicates the lives of so many men, with little indication when it’s present, a great deal of scientific research and funding has been done to improve the diagnostic process. Most recently, a team of engineers and scientists from Eindhoven University of Technology went to work on an ultrasound-based form of cancer diagnosis. Their goal was to eliminate the need for PSA tests altogether, because a false-positive PSA test may lead to painful biopsies down the road.
When cancer spreads through a person’s tissues, it produces large numbers of small blood vessels that proliferate in a highly specific pattern. The Eindhoven team used an injectable contrasting agent in their subjects to see these patterns, which can then be visualized on a computer screen. The whole process takes less than a minute. When they analyze their ultrasounds with actual cancerous prostates, they found dramatic similarities.
Up next for Eindhoven researchers is honing the process even more, so that other cancer diagnoses can benefit as well. “What we can do is translate this type of research toward other types of cancers that also need advanced diagnostic systems,” said lead researcher Massimo Mischi, “like for instance, breast cancer, which has the same incidence and the numbers of prostate cancer for women.”
In the meantime, the CDC urges all men to “take the time to decide” whether a prostate exam is worth the time and energy, based on their specific risk factors. You may just have a shy bladder. Or, you may be showing the early signs of a deadly disease. What’s important is knowing which information to consider when making your decision.

Published by Medicaldaily.com



























