New Personalized Cancer Treatment Administers Most Effective Drug Directly Into Tumor
Cancer treatment has always been a bit of a guessing game; there are over 100 drugs approved to treat cancer, yet choosing one of these drugs to help a patient toward remission is not an obvious decision. To eliminate the randomness in cancer treatment, scientists have turned their research toward personalizing cancer regimens. With the growing success of this course of specialized treatment for ovarian cancer patients, researchers at MIT are working to make specified treatment applicable to everyone, and their new device may be able to do just that.
In this new study, published in Science Translational Medicine, lead author Oliver Jonas, a postdoc at MIT’s Koch Institute for Integrative Cancer Research, describes this new device as very small in size (about the size of a grain of rice) but with the ability to do a lot of damage. The device can be implanted with a tumor and carry up to 30 different drugs at a time. After its implantation, the drugs can diffuse into the tumor tissue, allowing researchers to measure how effective certain drugs are over others at killing cells.
“You can use it to test a patient for a range of available drugs, and pick the one that works best,” Jonas said in a press release. By allowing doctors to see which drugs work best, this new device virtually eliminates the guessing element to cancer treatment.
For the most part, cancer drugs work by either damaging the DNA of tumor cells, or interfering with the cells’ functions. Nowadays, scientists are increasingly studying drugs that target tumor cells carrying a specific genetic mutation, but this research is often complicated by the unpredictability of whether a drug will work for a specific patient’s type of tumor.
To work around this complication, doctors have tried removing tumor cells from the source, growing them in a lab and treating them with different drugs to monitor effectiveness. This too has many drawbacks as removing tumor cells from their natural environments affects their growth and development, which ultimately affects how they will respond to drugs.
“The approach that we thought would be good to try is to essentially put the lab into the patient,” Jonas said. “It’s safe and you can do all of your sensitivity testing in the native microenvironment.”
The device, developed from a stiff, crystalline polymer, can be implanted in the tumor with a biopsy needle. Once the device is placed, different drugs release 200 to 300 microns into the tumor, without overlapping with each other. The device allows any sort of drug to be placed inside its reservoir, and researchers can manipulate doses delivered to tumor cells so that their drug regime is similar to what they would receive during a typical round of chemo via intravenous injection.
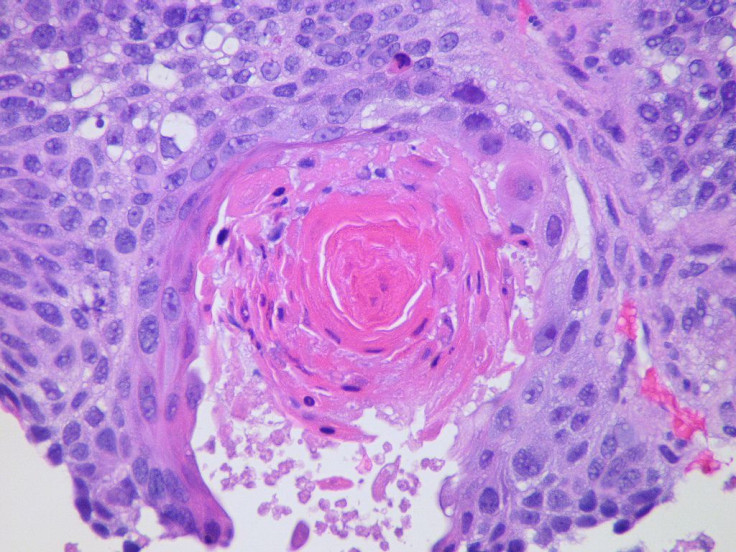
Once a day of drug exposure has passed, researchers remove the device and a sample of the tumor in the surrounding area to be tested. Using a stain with antibodies that can detect cell death or growth, researchers are able to analyze the tissue cells to see which drug doses were working.
Researchers first tested their device in mice grafted with human prostate, breast and melanoma tumors, all types of cancer known for having varying sensitivity to certain drugs. The researchers also tested their device on an aggressive type of breast cancer known as triple negative, which lacks the three most common breast cancer markers. Because of its missing markers, drugs often used to destroy this form of breast cancer do not target signifiers of genetic mutation, ultimately making treatment for patients with this disease an exclusively randomized process.
But once the device was implanted within triple negative tumors, results seemed to change. Doctors discovered that triple negative cells responded differently to five of the most common drugs used to treat this cancer. They were also able to isolate the most effective drugs as paclitaxel, doxorubicin, cisplatin, gemcitabine, and lapatinib, respectively. When administering these drugs through intravenous injection, they found the same positive results in tumor destruction, suggesting that this device is an accurate predictor of which drug works best.
Researchers also plan to use drug combinations, as the device is equipped to handle two or three drugs in the same reservoir, notes Jonas.
“This device could help us identify the best chemotherapy agents and best combinations for every tumor prior to starting systemic administration of chemotherapy, as opposed to making choices based on population-based statistics,” said Jose Baselga, chief medical officer at Memorial Sloan Kettering Cancer Center and co-author of the paper. “This has been a longstanding pursuit of the oncology community and an important step toward our goal of developing precision-based cancer therapy.”
Overall, researchers are very hopeful about their innovative treatment. They are continuing to improve their device, looking into ways to more easily read the device while implanted within the patient, and get the results more quickly. There is also the possibility that the device may be used in developing new cancer drugs for trials, and eventually widespread use. Most promising, though, is their plan to start a clinical trial for breast cancer patients, which will likely occur next year.
Source: Jonas O, Baselga J, Coombes C, et al. Drug testing in the patient: Toward Personalized Cancer Treatment. Science Translational Medicine. 2015.



























