Do Opioids Make Chronic Pain Worse? New Study Looks At Morphine, Oxycodone, And Other Prescription Meds
The opium poppy is arguably the oldest painkiller known to man, with its use being described by the ancient civilizations. Opium mimics the body’s home-made painkillers — endorphins and the like — and has given rise to the modern class of drugs called opioids that include morphine, fentanyl, methadone, and oxycodone. Opioids are very effective, and they remain the cornerstone of moderate to severe pain management.
Opioid prescriptions have dramatically escalated over the past few decades, a fact that has attracted significant media attention. With evidence-based medicine only becoming mainstream at the close of the 20th century, the science is still catching up on the long-term effects of opioids; older drugs like morphine have largely been grandfathered into modern medicine. Consequently, we’re still learning new things about this old class of drugs.
The latest finding is that opioids may actually worsen pain. My colleagues and I have just published a new paper in the Proceedings of the National Academy of Sciences showing that morphine can persistently exacerbate pain in rats. The medical community has recognized that opioids can cause abnormal pain sensitivity — termed opioid-induced hyperalgesia — but the sensitivity was only understood to occur while opioids were still present in the body. The surprising new twist is that morphine can increase pain for months after the opioid has left the body.
Pain lasted longer with morphine
We experimentally induced neuropathic pain — a type of chronic pain caused by damage or disease of nerves — in the rats by loosely constricting the sciatic nerve in the thigh. This created pain similar to sciatica. We measured pain in the rats by assessing their hind paw sensitivity to a poke from a plastic filament that is not normally painful. Once the neuropathic pain was fully established 10 days later, the rats received morphine or saline control (salt water) for five days via injections under the skin. From the injections, the drug circulates through the whole body.
As we expected, the neuropathic pain due to sciatic nerve constriction continued for another four weeks in the rats that had received the saline control. But for the rats that had received morphine, the neuropathic pain continued for 10 weeks. The five-day morphine treatment more than doubled the duration of neuropathic pain!
A separate experiment in the same study showed that morphine also worsened the neuropathic pain, an effect that lasted for more than a month after morphine treatment had ended.
We also showed that morphine did not have the same pain-promoting effects by itself — that is, when neuropathic pain was not present. A group of sham control rats underwent surgery, but the sciatic nerve was not constricted. The same five-day morphine treatment produced transient pain in these rats, but it lasted no longer than 24 hours. This means that long-lasting pain cannot be explained by morphine addiction or withdrawal, but by an interaction between morphine and the biological mechanisms underlying neuropathic pain.
How does morphine prolong pain?
To answer this question, we need to step back and discuss how chronic pain works.
If your hand is in harm’s way — on a hotplate, or under a falling hammer — this damaging event is detected by nerves in the skin and muscle. The nerves send electrical signals warning of danger to the spinal cord, and then up to the brain. The brain interprets the signal as "ouch" and sends another signal back down to move the hand away from danger.
When these nerves are damaged, several adaptations can occur, leading to painful sensations being exaggerated, and touch being misinterpreted as pain. Chronic neuropathic pain, which serves no useful purpose, occurs when these adaptations persist long after the original damage has healed. Why these adaptions persist and cause chronic pain in some people, but not others, is still not well understood.
This abnormal pain signaling has historically been viewed as an exclusive dialogue between nerves. But nerves only make up about 10 percent of the brain and spinal cord; the other 90 percent are glial cells — immune-like housekeepers that provide nutritional support for nerves, and clear away metabolic waste.
Research over the last two decades has shown that glial cells do much more than cook and clean. Glia recognize chemical signals from nerves, and respond by releasing chemical immune signals that influence communication between nerves. With abnormal pain signaling from nerves, glia respond by turning up the volume in spinal cord pain pathways. This results in the adaptations of painful sensations being exaggerated, and touch being perceived as pain.
As it so happens, opioids like morphine are also a chemical signal for glia. In our recent study, when morphine was administered in the presence of neuropathic pain, the glial cells went into overdrive. The glia released more immune signals, keeping the ‘pain volume’ turned up higher and for longer, than had they only been exposed to signals from the injured nerve. If the abnormal function of spinal glia was inhibited with drugs during morphine treatment, the pain was not prolonged.
This exaggerated glial response may also explain why some people develop chronic pain, but not others. Their glial cells may have been repeatedly stimulated with chemical signals — maybe morphine, or something else like an infection — to prolong pain from the initial injury.
Is this a death knell for opioids?
Our study is optimistic about the future of opioids in a clinical setting. By demonstrating that glial cell dysfunction is essential for morphine to prolong pain, we have identified a solution. Opioids achieve their desirable, pain-relieving effects by silencing nerves in pain pathways. Inhibiting the activity of glia with other drugs doesn’t interfere with pain relief; just the prolonged pain.
Research from my colleagues also suggests that inhibiting glia may eliminate other unwanted effects like addiction and tolerance, which leads to the need for ever increasing doses to achieve the same pain relief. Several labs are developing new drugs to inhibit glial dysfunction, which may improve the medical benefit of opioids.
The big picture and applications for humans
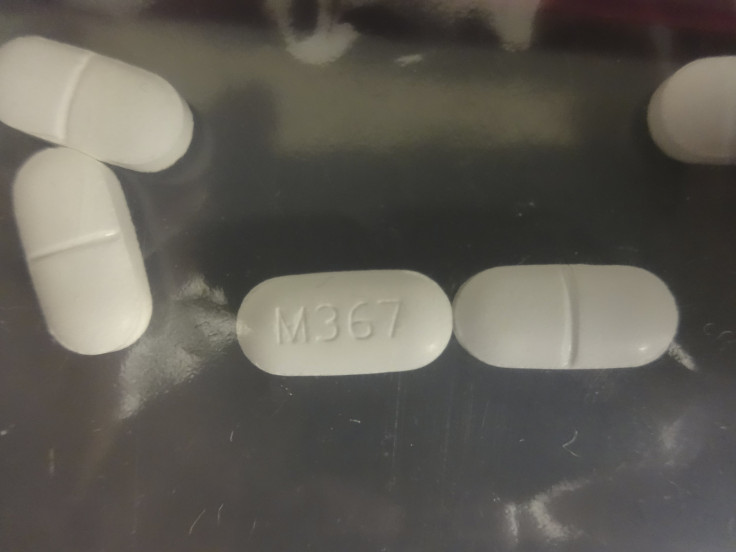
The recently published study focused on very specific conditions: neuropathic pain, morphine, a 10-day treatment lag, and male rats. Our latest results suggest that pain is still prolonged, even when these variables are changed. It holds up for other types of pain, like post-operative pain after surgery, if the treatment delay is shortened from 10 days, and occurs to a similar, if not greater degree in female rats. Similar effects are predicted for other opioids, like fentanyl and oxycodone, since they are also chemical signals for glia.
This study in rats has implications for humans. Our study is supported by troubling clinical reports that opioid use during surgery or for lower back pain is associated with subsequent chronic pain and increased disability. While opioids are the best painkillers available for the management of moderate-to-severe acute pain, the use of this drug class to manage pain lasting longer than a year does not have scientific support.
This study does not fill that gap in medical knowledge, but it should encourage clinical researchers to evaluate the long-term effects of opioids on pain. Better pain management is a goal worth striving for, and targeting glial cell dysfunction may be the answer.
Peter Grace, research assistant professor, University of Colorado
This article was originally published on The Conversation. Read the original article.



























