30% Of Prescriptions For Oral Antibiotics Are Unnecessary, Spurring Drug Resistance
The war against antibiotic resistance still has far too many doctors playing the role of Benedict Arnold, a new study published Tuesday in the Journal of the American Medical Association (JAMA) suggests.
Using the latest survey data culled from the Centers for Disease Control and Prevention (CDC), the researchers estimated the nationwide rate of antibiotic overuse among outpatient medical providers such as emergency department staff and primary care physicians from 2010 to 2011. Specifically, they examined how often doctors were prescribing oral antibiotics for medical conditions already known to rarely require the drugs because they’re either not caused by bacteria or are simply too mild to be worth the hassle. For some conditions, like inflamed sinuses or ear infections, they instead assumed the lowest prescription rates seen around the country represented the appropriate level of antibiotic use.
The researchers determined that at least 30 percent of the antibiotics prescribed by these doctors were unnecessary; for acute respiratory conditions, that percentage jumped up to 50 percent. Though these data are several years old, it’s likely the rates haven’t substantially improved since, according to lead author Dr. Katherine Fleming-Dutra of the CDC.
“Additionally, our estimate is a conservative estimate — we are focusing on instances in which no antibiotics were needed at all,” Fleming-Dutra told Medical Daily in an email. “We don’t consider the rest of inappropriate antibiotic use or misuse — for example, when an antibiotic is needed, but the wrong antibiotic is chosen, or the wrong dose is used, or the antibiotic is prescribed for too long or too short a time.” In other words, she added, “at least 30 percent of antibiotic prescribing is unnecessary, but the total amount of inappropriate use (overuse plus misuse) is probably much higher.”
Rather than focus narrowly on any one condition as earlier studies have, Fleming-Dutra and her colleagues wanted to grasp the full extent of antibiotic overuse — an effort directly sparked by the government’s recent pledge to cut the rate of overprescription in half by 2020. Judging from their findings, that will take trimming 15 percent, or 23 million, from the estimated 154 million prescriptions doled out by doctors annually.
It’s a task easier calculated than done, given that widespread public health efforts to encourage restraint with antibiotics seem to have fallen on deaf ears. Some of this failure, Fleming-Dutra said, can be chalked up to doctors’ unwillingness to alienate their patients: "In studies, clinicians report that concern about patient satisfaction and demand for antibiotics sometimes drives them to prescribe antibiotics when they shouldn’t.”
The answer to these concerns isn’t a hastily scribbled prescription note so much as it is a better doctor-patient relationship, she said. “Regardless of their expectations, the majority of patients trust clinicians to recommend the right treatment. If antibiotics are not needed, most patients will be satisfied without antibiotics if the clinician can communicate why an antibiotic is not needed, what the patient can do to feel better, what to expect with their illness, and when they should come back if they are not getting better or are getting worse.”
Of course, there’s plenty that can be done to educate patients as well. “Both clinicians and patients need to understand that antibiotics aren’t always the answer,” Fleming-Dutra said. “Sometimes antibiotics can cause harm too, such as in the case of side effects, allergic reactions, and Clostridium difficile infection, the sometimes deadly diarrhea.”
Some practical steps towards combatting antibiotic overuse, as highlighted by an accompanying editorial in JAMA, can include putting up informational posters in patient waiting rooms and keeping in touch with primary care providers four times a year following a one-hour educational session on the topic.
However we get there, the team hopes their findings can at least help doctors, public health officials, and potential patients better understand the gravity of the situation.
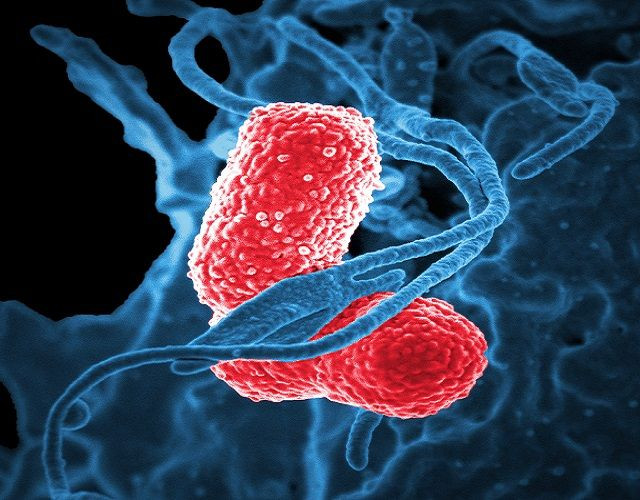
“Antibiotics are life-saving medicines, and antibiotic resistance is one of the most urgent public health threats of our time. The CDC estimates that each year in the United States, 2 million people are infected with antibiotic-resistant bacteria and 23,000 people die from antibiotic-resistant infections,” Fleming-Dutra said. “Simply using antibiotics creates resistance, and that’s why it is critical to use antibiotics only when needed and, if needed, use them correctly.”
Source: Fleming-Dutra K, Hersh A, Shapiro D, et al. Prevalence of Inappropriate Antibiotic Prescriptions Among US Ambulatory Care Visits, 2010-2011. JAMA. 2016.



























