Precision Medicine Exposes Patients' Genetic Information; Sharing And Protecting Data With Google

Since the completion of the Human Genome Project in 2003, medical science has struggled with how best to use genomic testing to customize an individual’s health care. There is a palpable excitement about the possibility that comes from unearthing genomic differences among people and diseases that we didn’t know about just a few years ago. But the dialogue around precision medicine has also been rife with apprehension, ethical queries, and unanswered questions.
Most medical treatments are designed for the average patients with a one-size-fits-all approach. The Precision Medicine Initiative has the potential to revolutionize the way doctors diagnose, treat, and prevent diseases and designed personalized health care. Recognizing the promise genomic sequencing could have, the White House has allocated a $215 million investment into the ambitious new research initiative announced earlier this year.
The budget will pay for the National Institutes of Health to assemble at least one million study participants, sequence their genomes, identify genes linked to cancer and disease, and process, organize, and protect their vastly cumbersome personal data. One of the challenges will be ensuring that the data collected will be harnessed and used for good, without exposing patients to serious breaches of privacy.
“For these million people who are going to consent to say, ‘I’m going to be among the first in the country to give all of this data to science,’ we have to be very cognizant of this and need to build in lots of privacy protections,” said Dr. Eric Green, director of the Human Genome Research Institute. “We want anybody who’s a qualified researcher access to that data, but at the same time we need to build in appropriate protection so it’s not abused. We have to decide as a society what is and isn’t going to be acceptable in terms of how people use and access data.”

In 2008, experts were able to foresee a need for protecting genomic information, giving birth to GINA. The Genetic Information Nondiscrimination Act is a federal law that protects Americans from being treated unfairly by employers and health insurers because of differences in their DNA. It also enables patients to take part in research studies without having to worry if their genomes will be used against them through insurance penalties or discriminations in the workplace.
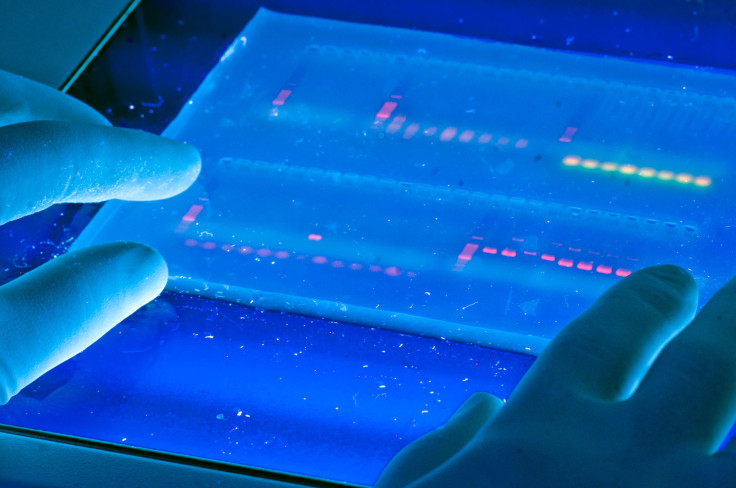
At the time the president signed the act into law, whole genome sequencing was reserved only for those who had advanced forms of cancers or patients with mysterious diseases suspected to be caused by genetic mutations. They were the kind of patients who were treated with drugs that failed, leaving them with no alternative plan except to have doctors take a closer look inside their genes for possible solutions. Since then, costs have since shrunk dramatically, and now labs are on their way to being able to sequence nearly every cancer patient who walks into the oncologist’s office.
“Almost every single cancer now is looked at under a microscope by a pathologist as a key part of deciding what kind of cancer somebody has and how severe it is,” said Dr. Eric Green, director of the Human Genome Research Institute (HGRI). “I believe in the next five years that [for] many, if not most, types of cancer, the pathologist will be analyzing the genomic sequence, and then there will be a fingerprint of genomic information about that cancer.”
That enormous amount of data needs to be implemented for use in a research setting and accessible on a shared network to both doctor and patient. Putting a system in place to collect, store, and analyze the data of a new generation will be a feat in itself. Current computers can’t keep up with the rapid accumulation of sequenced genomes, forcing researchers to rethink how to design software powerful enough to handle the next-generation of sequencing, according to a study published in the journal Nature Methods.
“The volume of data that’s produced through genome sequencing can’t fit into a patient’s record,” said Dr. Richard Sharp, director of the Biomedical Ethics program at Mayo Clinic. “It’s terabytes of data. If it doesn’t go into the health records, then the question is where does it sit? Where do we store that information for us to reanalyze the data as we learn more?”
Sharp points out that we need a system that will have security measures in place comparable to the protections currently given to today’s traditional health records — but one that also gives institutions access to the data they need to help identify links between diseases and genes moving forward. Companies are already trying to fulfill that demand.
A Google Cloud of Genomes
For just $25 a year, Google will store your genome in the cloud. In March 2014, the search engine giant launched “ Google Genomics,” offering hospital and universities the ability to store a patient's complete set of genetic material, all 100 gigabytes of it. Seeing the value, the National Cancer Institute decided to fund $6.5 million toward storing cancer-specific genomic information onto the cloud in order to make it available to anybody worldwide. The ultimate goal is to create “cancer genome clouds” for scientists to share information and expedite virtual experiments.
“We saw biologists moving from studying one genome at a time to studying millions,” David Glazer, the software engineer who led the effort and was previously head of platform engineering for Google+, told MIT Technology Review. “The opportunity is how to apply breakthroughs in data technology to help with this transition.”
By creating an interface to connect and compare genomes by the thousands and millions, Google has enabled researchers, doctors, patients, and parents to search for answers to medical anomalies through a shared database. They’re not the only company to have realized the need for a shift in medical technology. Amazon, IBM, and Microsoft have already established teams of bioinformatics experts to design computer systems competent enough to compete with Google.
Using one of the fastest pieces of computing equipment at Broad Institute in Cambridge, Mass., laboratories are able to decode DNA at a rate of one genome every 32 minutes. That translates to approximately 200 terabytes of raw data, exceeding the amount most biologists have ever handled. The data flow won’t stop there. Collecting sequenced genomes is only a piece of the Precision Medicine Initiative.
You are more than just your genome. Humans are the environment they grew up in, the family and friends they socialize with, the drugs and alcohol they consume or abstain from, the physical activity they engage in, and the foods they eat and drink. Tracking day-to-day information is equivalent to sequencing the human genome, making “mHealth” technologies another key piece of the puzzle.
Already, Fitbits, mobile tracking devices and other wearable sensors are empowering patients to monitor different aspects of their physiology like counting the steps they’ve taken, measuring the nutrition from foods they’ve eaten, and, for diabetics, managing glucose levels. But in the near future, researchers should be able to organize, process and analyze all this genetic and environmental data in order to make an all-encompassing assessment and better tailor medical care.
“Think about where sequencing was 10 years ago, that’s probably where the Fitbit is today,” Green says. "The amount of money and energy currently being invested into developing wearable sensors and monitoring technologies will pay off in the form of information. Fitbits are the start of a technology revolution that will really empower people to collect information about themselves, not just for fun but for their individualized care.”
DNA On Demand
MHealth technologies provide potential platforms for researchers to aggregate large sums of information on entire populations over time. Consider the possibilities of getting a direct data stream from the 285 million-plus mobile phone users in the U.S., for example.
Imagine DNA sequencing for your iPhone. Maybe one day we’ll be able to say there’s an app for that, but right now we’re at the pivot point. The medical community holds in their hands the technological equivalent to their first computer model, representing the possibility of new dominance over the human body and disease.
“Precision medicine initiative hopes to tackle head on,” Green said. “If you have an incredible amount of data from a million people there’s no question you could learn a lot, but the hurdle is not getting the data, it’s going to turn out to be analyzing the data. This will be the bottleneck; it already is and will continue to be.”
Biomedical research is in transition, converging together technology innovation in genomics with mHealth trackers, allowing doctors to generate a mass capacity of data. Accumulating information is only as valuable as the way in which sophistication can allow it to be analyzed and integrated.
“Here’s where things get complicated,” said bioethics expert Dr. Richard Sharp, director of the Biomedical Ethics program at Mayo Clinic. “You’re then sending medical information into an electronic health record and that information is then coming from a source that is difficult to verify — is it you or your kid wearing your Fitbit? Similarly, is your glucose fasting level going out to you or is this information going out to a place where information is shared? This could lead to some serious privacy issues where disseminating medical information using these devices.”
Genetic discrimination in the workplace or through insurers was one of the earliest fears expressed when the first genome was sequenced. When the President signed GINA, it turned genetic information into a nationwide goal that would encourage trust in the sequencing system and protect genomes before they’re sequenced. Aside from putting federal laws in place to protect the public, creating competent systems will be a futuristic hurdle. Fearing email hackers will become a juvenile antiquated stunt compared to those stealthy enough to gain access into a person’s genomic information.
But Sharp also thinks his two-year-old bioethics department could work through the privacy concerns. Mayo Clinic established a national advisory group of experts in law and medicine throughout the country in order to predict and assess risk any new and potentially transformative technology might bring to public health.
“We need to be sure that whatever these mhealth apps become, we’re thinking very creatively about that future and we’re not just going to wait, see, and manage the issues as they come,” Sharp said. “These do feel like technologies — the mhealth and genomic testing — are going to be transformative in some way and cause us to engage medicine and medical care in very different ways.”
Published by Medicaldaily.com



























