Risk Of Alzheimer’s Disease Doubles In Presence Of Specific Gene Variants, Motivating Early Treatment
Human DNA may contain key genetic variations that, when present, substantially increase a person’s risk for developing Alzheimer’s disease, according to a new study published in Nature.
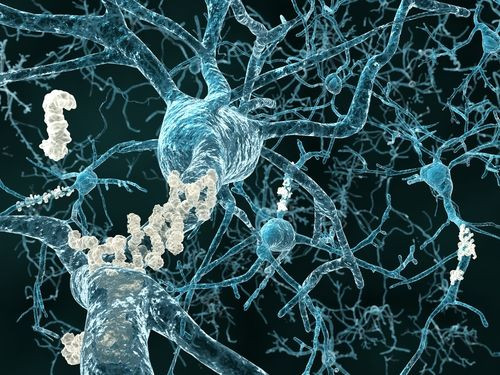
After analyzing more than 15,000 cases of people with and without Alzheimer’s, researchers from Washington University in St. Louis discovered that the phospholipase D3 gene (PLD3), when inactive, results in a marked increase in beta-amyloid production. A protein manufactured in the brain, beta-amyloid is one of the disease’s hallmarks, as it gets converted in disruptive plaques that make communication between neurons difficult, eventually killing the neurons themselves. Now that scientists have discovered the gene’s effects, treatment options may become more attractive to people who face an increased risk, yet show no signs of the disease.
Roughly 5.2 million Americans lived with Alzheimer’s in 2012, with approximately one in eight older Americans suffering from the neurological disorder. As the most common form of dementia, Alzheimer’s is the sixth-most common cause of death in the United States, according to the Alzheimer’s Association.
“We were very excited to be able to identify a gene that contains some of these rare variants,” lead author Carlos Cruchaga, at the university’s School of Medicine, said in a news release. “And, we were surprised to find that the effect of the gene was so large. After adjusting for other factors that can influence risk for the disease, we found that people with certain gene variants were twice as likely as those who didn’t have the variants to develop Alzheimer’s.”
Initially, Cruchaga and his colleagues sequenced all the protein-coding genes from several individuals in each of the 14 families. The process involved in this sequencing is known as whole exome sequencing, and it’s essentially a cheaper, more efficient sampling than relying on the entire genome. Some of the family members involved in the study had Alzheimer’s, while others did not. The researchers compared the genes of both groups and discovered PLD3 remained present in the same variation in people carrying the disease.
“We then studied another 11,000 other people with and without the disease and found that a PLD3 gene variant doubled the risk for Alzheimer’s disease,” explained Cruchaga. “This PLD3 variant, like the recently identified rare variant in the TREM2 gene, appears to confer more risk for Alzheimer’s disease than other genes identified by the latest genome-wide association studies.”
Also important, notes researcher Alison Goate, is the methodology used to identify these genes. Rather than pooling from a random sample, using data from members of the same family allowed the research team to draw definitive links between the variants. “The approach we’ve taken in this project is just as important as the discovery that this gene is involved in Alzheimer’s,” said Goate. “By studying gene variants within families, we were able to narrow down the number of variants that might cause disease. If we had been using unrelated individuals, we would not have had the statistical power to find these rare variants.”
Unfortunately, like much of Alzheimer’s, the exact mechanism for activating or deactivating the gene is still a mystery. So far, researchers have only succeeded in observing the variation’s effects on beta-amyloid production. This much, however, is sufficient to running future tests on the PLD3 gene, as the specific function of a gene is less important than its actual effects, Goate explains.
“But now that we’ve found that this gene is involved,” she added, “we need to figure out its precise role in the body and how particular variants contribute to the development of Alzheimer’s disease.”
Source: Cruchaga C, Karch C, Jin S. Rare coding variants in the phospholipase D3 gene confer risk for Alzheimer’s disease. Nature. 2013.



























