Schizophrenia Treatment Restores Neural Connections, Reverses Memory Loss In Mice
One of schizophrenia’s most difficult symptoms to treat is memory loss, but scientists have now successfully reversed memory loss in mice with the mental health disorder, according to new research that may provide hope of new treatments for the more than 21 million people worldwide with schizophrenia.
The discovery, built on decades of research, was accomplished by disrupting a genetic chain of events that causes abnormal lack of growth of neurons in the brain’s memory center. Scientists at Columbia’s Mortimer B Zuckerman Mind Brain Behavior Institute, Columbia University Medical Center (CUMC), and the New York State Psychiatric Institute (NYSPI) regrew connections between these brain cells in mice by using a chemical compound, which subsequently restored the memory deficits.
"With these findings, we showed that restoring cellular connections reversed memory deficits — a symptom of schizophrenia for which there is no effective treatment,” said Dr. Joseph Gogos, a principal investigator at the Zuckerman Institute, in a press release. “This represents an invaluable new strategy for treating schizophrenia and highlights the critical importance of basic biological research in psychiatric disorders. Understanding how schizophrenia originates in our model lends critical insight into the disorder as a whole, paving the way for improved treatment options that have thus far remained elusive.”
Hallucinations, paranoia, and delusions are the most well-known symptoms of schizophrenia, and can often be treated by antipsychotic medications. Severe disruptions to short-term and verbal memory, however, have remained largely untreatable along with other symptoms, such as reduced attention and a decrease in IQ. Memory deficits have the power to cut a person off from the world around them by making it difficult to maintain a job or relationships, according to the release.
“Memory deficits are now considered a core feature of schizophrenia and are believed to be strongly tied to the disorder’s underlying biology,” explained Dr. Joshua Gordon, associate professor of psychiatry at CUMC. “Until we can shed light on that biology, these symptoms remain virtually impossible to treat.”
Gogos has worked to uncover these biological bases for almost 20 years. He and his colleagues developed a mouse model of schizophrenia with a specific gene mutation, known as the 22q11.2. The mutation is the single largest genetic risk factor for the disease.
“Schizophrenia affects about one in every 100 people, but for those with a 22q11.2 microdeletion, that chance jumps to one in three,” Gogos said. “22q11.2 microdeletions remain the single greatest genetic risk factor for developing schizophrenia. This is why our model has proved invaluable in allowing us to trace schizophrenia back to its beginnings.”
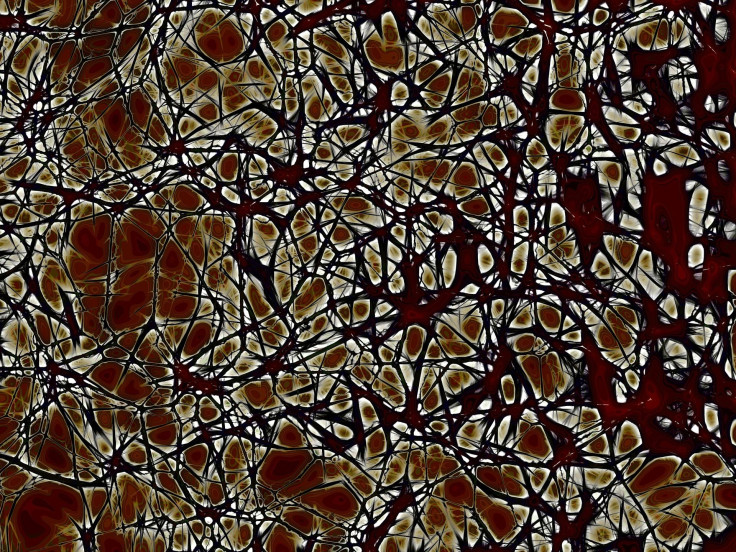
The research team released a study last year explaining how a 22q11.2 microdeletion leads to weaker connections between neurons and important brain regions. Normally, Gordon said, neurons grow long branches that extend across long distances and form interconnected units. In the mouse models used in the experiment, the branches were stunted in the prefrontal cortex and hippocampus — two brain regions that are key to memory. Further experiments revealed an abundance of the protein Gsk3β had clogged up the brain. For the current study, the team tested whether suppressing the protein’s activity could reverse the damage that leads to memory deficits.
They found that as Gsk3β activity was blocked, neurons branched out and began forming connections with their neighbors. Communication between regions was restored and most importantly, the mice showed no memory deficits.
“Our work suggests that Gsk3β could be considered a potential target for treating some symptoms of schizophrenia — though there are limitations,” Gordon said, “for example, whether the same treatment might work in other models of schizophrenia that do not have the 22q11.2 microdeletion. Also, we treated the mice at a young age, but schizophrenia normally presents in adolescence and young adulthood.”
The researchers plan to test whether blocking Gsk3β at an equivalent age would have the same positive effect.
Source: Gordon J, Gogos J, Tamura M, Mukai J. developmental inhibition of Gsk3b rescues behavioral and neurophysiological deficits in a mouse model of schizophrenia disposition. Neuron. 2016.



























