Scientists Coax Stem Cells Into Functional Red Blood Cells, Taking Us Closer To Limitless Artificial Blood
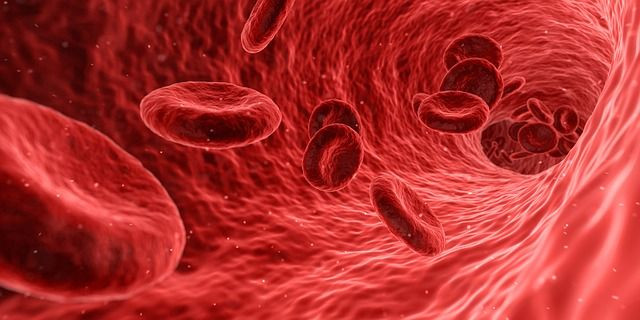
Blood is one of the most vital components of the human body, but we can't create an artificial version, which means we must rely on donations for transfusions and operations. However, two recent studies suggest we're closer than ever to making a limitless, articifial supply of blood.
In one new study, researchers created a mix of different types of blood stem cells that produced different kinds of human blood cells when transfused into mice, The Independent reported. This is an important step toward making artificial human blood, as doctors believe that figuring out a way to turn stem cells into blood artificially will eventually lead to this breakthrough.
“This work is the culmination of over 20 years of striving,” explained study researcher George Daley, The Independent reported. “We’re now able to model human blood function in so-called ‘humanized mice’. This is a major step forward for our ability to investigate genetic blood disease.”
Stem cells are cells that can essentially transform into any type of cell. While we have been able to stimulate these stem cells into becoming blood cells in the past, this has only been on levels too small to be used in a medical setting. For example, in a study published in March, scientists in England were able to produce about 50,000 red blood cells by coaxing stem cells into transforming into red blood cells. However, according to The BBC, the average bag of blood contains about a trillion blood cells.
Another problem that stands in our way of successfully making limitless artificial blood is the risk of these new blood cells becoming cancerous, The Independent reported. One of the key traits of blood is that it is able to “self-renew” and create more of itself, but unfortunately this is also a key trait of tumors.
In a second study, researchers at Cornell University in New York were able to create artificial mouse blood, and then successfully infuse living mice with this blood. When the mice’s immune system was removed, the artificial blood was able to reproduce immune blood cells. This finding hints that artificial blood could also help to treat patients with a range of immune disorders.
For now, these studies have only been conducted in animals; scientists are still not ready for human testing, so we still need human donations. According to the American Red Cross, someone is in need of a blood donation every two seconds, and about 36,000 units of red blood cells are needed everyday. Although an estimated 38 percent of the U.S. population is eligible to donate blood at any given time, less than 10 percent of that eligible population does each year.
Source: Sugimura R, Jha DK, Han A, et al. Haematopoietic stem and progenitor cells from human stem cells. Nature . 2017
Lis R, Karrasch CC, Poulos MG, et al. Conversion of adult endothelium to immunocompetent haematopoietic stem cells. Nature . 2017
See Also:



























