Sickle Cell Anemia Treatment; UI Health Finds Transplants Can Cure Sickle Cell Without Chemotherapy
With 70,000 people in the United States having sickle cell disease and 1,000 babies born annually with the debilitating disorder, scientists are hard-pressed to find a cure. Researchers at the University of Illinois Hospital and Health Sciences System are getting close, however. In a second phase clinical trial, a team of physicians has successfully cured 12 adults by using stem cell transplants from sibling donors. Finding much hope in their continued success, they published their study in the journal Biology of Blood and Marrow Transplantation.
The procedure originated at the National Institutes of Health campus in Maryland, where 30 patients were treated, resulting in an 87 percent success rate. Physicians at UI Health advanced this research in phase 1 and 2, where 92 percent of those treated were cured of the disease.
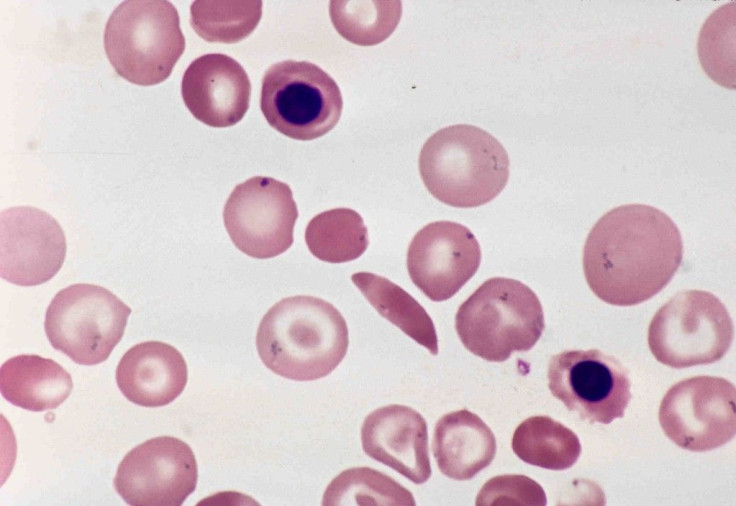
Finding cures that go beyond treatment to improve quality of life is crucial for many different reasons. Right now, sickle cell disease, a genetic disorder, affects one in every 500 African-Americans in the United States. The disorder causes red blood cells to become misshapen, taking on a sickle-like appearance as opposed to the circular shape of a healthy cell. As a result, red blood cells, which are essential in carrying oxygen, can get caught on one another, especially while passing through smaller blood vessels. When this happens, the oxygen cannot be delivered to body tissues, resulting in pain, organ damage, and possibly stroke.
Doctors have long known that bone marrow transplants offer the possibility to cure sickle cell disease. But when adults receive these transplants, they also need to undergo high-dose chemotherapy to prevent their own cells from growing back, as well as keeping the immune system from attacking the new cells. Chemotherapy isn’t necessary with this new treatment, however, making it suitable for patients who couldn’t risk undergoing chemo.
“Adults with sickle cell disease are now living on average until about age 50, with blood transfusions and drugs to help with pain crises, but their quality of life can be very low,” Dr. Damiano Rondelli, chief of hematology/oncology at UI Health, said in a press release. “Now with this chemotherapy-free transplant, we are curing adults with sickle cell disease, and we see that their quality of life improves vastly within just one month of transplant.”
For this treatment, doctors first administer immunosuppressive drugs to patients in conjunction with a low dose of total-body irradiation to prevent the new cells from being rejected. Then, donor cells taken from a healthy sibling are given to the patient through a transfusion. These stem cells eventually lead to the production of more healthy cells for the patient. As a result, symptoms associated with the disorder are often relieved, and patients told to continue taking immunosuppressants for the next year.
For the second phase, researchers gave 13 patients between the ages of 17 and 40 transplants from their sibling. In order to find if the sibling was a close match, researchers tested both the potential donor and the sibling for human leukocyte antigens (HLA) markers found on these cells. To be deemed a match, the donor had to have 10 of the same HLA markers as the patient.
Going beyond the NIH research, the team was even able to transplant cells from a donor into patients who didn’t have the same blood type, but matched for HLA markers. They also found that none of their patients showed signs of graft-versus-host disease, which results when immune cells from the donor attack the recipient’s cells.
Examining their patients a year later, researchers found that 12 of the transplants were a success, and these patients reported having less pain and better quality of life. Four of these patients were even able to stop immunotherapy before the year was up, without complications or rejection of donor cells.
“Adults with sickle cell disease can be cured without chemotherapy — the main barrier that has stood in the way for them so long,” Rondelli said. “Our data provide more support that this therapy is safe and effective and prevents patients from living shortened lives, condemned to pain and progressive complications.”
Source: Saraf S, Oh A, Rondelli D, et al. Non-Myeloablative Stem Cell Transplant with Alemtuzumab/Low Dose Irradiation to Cure and Improve the Quality of Life of Adults with Sickle Cell Disease. Biology of Blood and Marrow Transplantation. 2015.



























