Sickle Cell Drug, Hydroxyurea, Shown To Reduce Symptom Severity And Healthcare Costs
The genetic condition of red blood cells bending and clumping, known as sickle cell disease, has been treated with the drug hydroxyurea with success since the early 1990s. Now, new data shows the drug’s efficacy in reducing the life-threatening symptoms can also cut healthcare costs associated with the disease’s treatment.
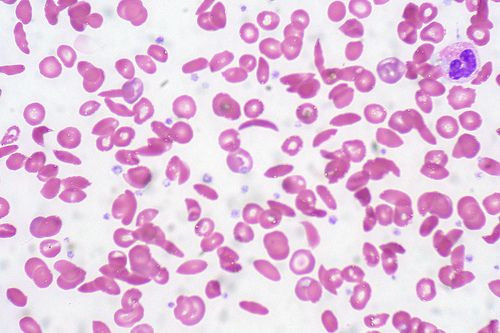
Due to the disease’s characteristic effect of bending red blood cells into C-shapes, or “sickles,” patients who suffer from the disease face a far greater risk of stroke and blood clots, as the cells can accumulate inside blood vessels and block circulation. Hydroxyurea’s ability to restore safer levels of hemoglobin, thus “re-inflating” the cells, has been shown in a recent study to reduce overall costs due to fewer serious respiratory problems and pain crises that require blood transfusions and other treatments.
“In addition to alleviating the human suffering in sickle cell disease, we found that hydroxyurea had the pleasant ‘side effect’ of substantially lowering the cost of care among children treated with it,” study investigator James Casella, M.D., director of pediatric hematology at the Johns Hopkins Children’s Center, said in a press release.
Casella and his colleagues reviewed the number and cost of hospitalizations among 167 sickle cell patients, ages 1 to 3, treated at three pediatric hospitals between 2003 and 2009. Fifty percent of patients received hydroxyurea in addition to their standard pain medications and regular blood transfusions; the other half received only standard care and a placebo. The researchers believe their study is the first of its kind to perform a cost-benefit analysis of hydroxyurea.
Bolstering the drug’s proven effectiveness, children who took hydroxyurea were hospitalized 232 times compared to the control group’s 324 times. Researchers also found the total cost associated with the drug’s treatment was lower — despite the outpatient costs being slightly higher. The average cost of hospitalization for hydroxyurea patients was $9,450, while the other group paid $13,716 on average. Adjusted for the greater outpatient cost, the total difference between the drug and the placebo was $11,072 to $13,962, respectively.
“Our analysis specifically demonstrates an added benefit to the use of hydroxyurea for treatment of sickle cell disease related to the drug’s impact on the cost of medical care,” said the study’s lead investigator Winfred Wang, M.D., of the Hematology Department at St. Jude Children’s Research Hospital, “and should be another factor in support of more widespread use of the drug in both children and adults.”
Sickle cell disease is passed along genetically and is most common among people of African, Mediterranean, Middle Eastern, and Hispanic descent. Roughly 100,000 people in the United States have sickle cell disease, according to the news release. In addition to hydroxyurea, popular treatment options include antibiotics such as penicillin — which children take as early as 2 months, until they’re 5 years old — and over-the-counter pain relief medications, as the buildup of red blood cells in the vessels is often extremely painful.
In the event that certain medications fail, doctors will perform a series of blood transfusions to replace the defective red blood cells with a batch of healthy ones. These carry the risk of overloading a patient’s body with iron, for which he or she would have to take certain medications, such as deferasirox (Exjade), to treat.
The latest study has researchers feeling optimistic about the drug in future use, especially as it is the only one currently approved by the Food and Drug Administration to treat sickle cell disease. Lower overall costs mean greater access to the drug and fewer instances of hospitalization due to undue complications.
“Our main goal is to find better treatments,” Casella said. “But in a time when we are trying to curb health care spending while improving patient outcomes this is really welcome news.”
Published by Medicaldaily.com



























