Staph Skin Infection Myths: What You Believe About Antibiotics Is Wrong


The question originally appeared on Quora. Answer by Drew Smith.
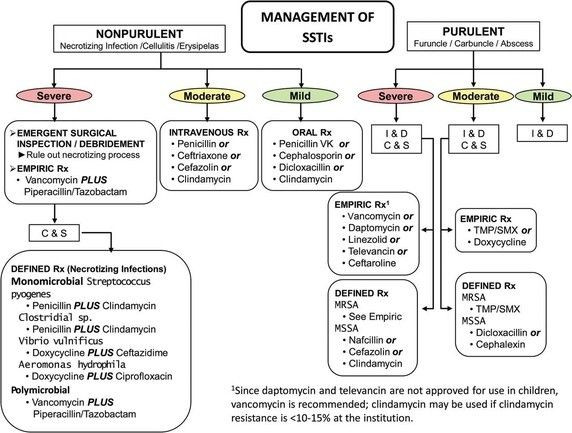
Antibiotics are not especially effective in treating skin infections. This is true for both topical and systemic antibiotics [1] [2] [3] [4] [5] . Incision and drainage is typically just as effective in treating uncomplicated infections. However, antibiotics are routinely prescribed for skin infections, in accordance with IDSA guidelines: [6]
Why are they prescribed if they are not very effective? Because they reduce the risk of systemic infections.
Not everyone holds the view that antibiotics do little to help heal infected wounds. Brad Spellberg argues that most modern trials of antibiotic effectiveness are too small to detect small but clinically significant effects of antibiotics [7] . He bolsters this argument by analyzing the pre-1950 literature, when placebo-controlled trials of antibiotics were much more common [8] . Cure rates for infected wounds and ulcers were 36% in untreated/placebo groups vs 83% for penicillin-treated groups, for example.
That’s a pretty big effect, and it raises the question of why we don’t see such big differences today. I can think of a few possible explanations:
- The pre-1950 cure rate with penicillin is not that different than the modern cure rates for placebos. I suspect that modern medical practice and perhaps improved social/environmental conditions lead to better outcomes independently of antibiotics. It’s not that antibiotics are ineffective, rather they are superfluous in treating patients who were going to get better anyway.
- Perhaps penicillin is uniquely effective in treating wounds. Tissue penetration is a big factor here: wounds are typically poorly perfused and systemic antibiotics may never attain therapeutic levels. Penicillin has very good tissue penetration properties and so may attain higher levels in wounds than other antibiotics. But since 1950, nearly all strains of S. aureus have become penicillin-resistant, and penicillin is no longer prescribed for skin infections.
- More subtly, bugs may have evolved to wall themselves off better from antibiotics. Many pathogenic bacteria, including S. aureus have “clumping factors” which create fibrin deposits around the wound. These deposits inhibit infiltration by neutrophils and macrophages and also reduce perfusion by antibiotics. Bacteria may have increased their ability to create effective physical barriers that wall themselves off from antibiotics.
Although Spellberg’s objections are well-considered, they may not be relevant for current medical practice. Antibiotics are just not as effective in treating skin infections as one might believe.
Footnotes
- [1] Randomized, controlled trial of antibiotics in the management of community-acquired skin abscesses in the pediatric patient.
- [2] Randomized, double-blind, placebo-controlled trial of cephalexin for treatment of uncomplicated skin abscesses in a population at risk for communit... - PubMed - NCBI
- [3] The treatment of acute superficial abscesses: a prospective clinical trial.
- [4] Treatment of cutaneous abscess: a double-blind clinical study.
- [5] Randomized controlled trial of trimethoprim-sulfamethoxa
zole for uncomplicated skin abscesses in patients at risk for community-associated methicil... - PubMed - NCBI - [6] Practice Guidelines for the Diagnosis and Management of Skin and Soft Tissue Infections: 2014 Update by the Infectious Diseases Society of America
- [7] To treat or not to treat: adjunctive antibiotics for uncomplicated abscesses.
- [8] Antimicrobial agents for complicated skin and skin-structure infections: justification of noninferiority margins in the absence of placebo-controll... - PubMed - NCBI
More from Quora:
Published by Medicaldaily.com



























