Ultrasound Therapies Restore Memory In Alzheimer's Mouse Models
Using ultrasound waves, a team of Australian scientists have successfully eliminated from mouse brains the damaging beta-amyloid proteins thought to cause Alzheimer’s disease. Though far away from human models, the discovery opens new doors for conquering the largely misunderstood illness.
The more science learns about dementia, the less power it seems to wield. Alzheimer’s disease has shown no sign of stopping ever since it was first discovered in the early 20th century, and only recently have neurologists been able to peek inside subjects’ brains to learn where malfunction occurs. Ultrasound therapies stand as the most cutting-edge techniques currently available, as they rely on the skull’s blood-brain barrier to target harmful protein clumps at the source.
Neuroscientist Jürgen Götz, together with graduate student Gerhard Leinenga of the Queensland Brain Institute, published the findings of their recent study in Science Translational Medicine. In their research, they found mice with abnormal clumps of the Alzheimer’s-like protein regained lost memory and cognitive function when Götz and Leinenga exposed the animals’ brains to repeated scanning ultrasound (SUS) treatments. The technique relies on creating tiny leaks in the barrier between the brain’s own ecosystem and the rest of the body, and using microbubbles to clear out unwanted neural “garbage.”
After a period of six to eight weeks, the team tested the mice on their ability to navigate a maze, recognize objects, and detect areas they should avoid. The mice who had received only microbubble injections showed no improvement in their cognitive tasks. Meanwhile, the mice whose brains had been made permeable with SUS demonstrated improved ability on all three. What’s more, the overall plaque burden was cleared away in 75 percent of the mice given SUS.
The discovery builds on prior success published in Radiology last year. Led by SUS’s originator, Dr. Kullervo Hynynen of the Sunnybrook Research Institute in Toronto, a group of researchers arrived at a similar conclusion using MRI-guided ultrasound waves to the hippocampus — a key area in the brain for studying Alzheimer’s. The technique yielded reduced abnormal activity from amyloid proteins and increased plasticity of the brain cells. Speaking to Science, Hynynen said that if the findings could be translated from mouse to human models, “it will revolutionize the way we treat brain disease.”
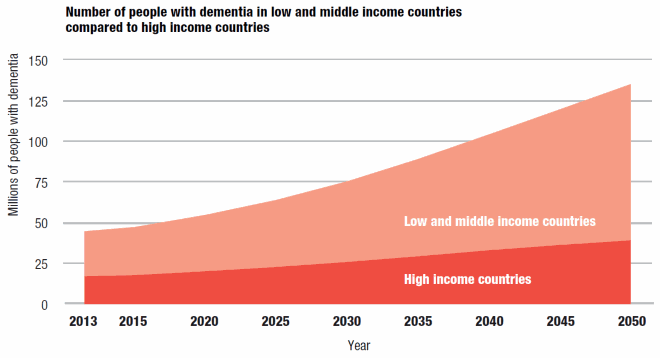
In 2013, 44.4 million people were living with dementia worldwide. By 2030, Alzheimer’s Disease International estimates that figure will rise to 75.6 million, and by 2050, 135.5 million. People are living longer, and medical science is getting better at treating physical illnesses with medication. But increased longevity is now giving way to the negative effect of brain disorders, for which we have yet to develop any treatments.
Using ultrasound waves to clear out beta-amyloid plaques may not be the panacea scientists hope for. Mouse models are reliable indicators for many physical dysfunctions, but human brains are far more complex. And any quirks of chemical imbalance may get exploited as researchers move up the food chain, particularly as deeper forms of memory loss and behavioral deficits begin to crop up.
Nevertheless, early wins mean the studies can stay on their course. Hynynen is working toward getting commercial approval of the ultrasound technique and says all of the testing to-date has yet to produce a negative effect in animals. Brian Bacskai, a neurologist at Massachusetts General Hospital, has visions even further down the line.
“Imagine if your grandmother went to the clinic once per year, and it cleared beta-amyloid and that was all it took — no surgery, no drugs,” he told Science. “It would be amazing.”
Source: Leinenga G, Götz J. Scanning ultrasound removes amyloid-β and restores memory in an Alzheimer’s disease mouse model. Science Translational Medicine. 2015.



























